In medical practice, accurate assessment tools are crucial for diagnosing neurological conditions, especially when dealing with stroke patients. These assessments help determine the severity of symptoms and guide treatment plans. Understanding the process and scoring system is essential for healthcare professionals to provide effective care. This section delves into a widely used set of criteria for evaluating neurological impairment, focusing on the most recent updates and how they impact clinical practices in 2025.
Important Updates in Stroke Evaluation
The methodology for evaluating stroke symptoms has evolved over time, incorporating new research and clinical experiences. These updates ensure that assessments remain relevant and accurate in diagnosing various types of brain injuries. Changes in the criteria and scoring system help healthcare providers make more informed decisions about patient care, leading to better outcomes.
Key Modifications in the Scoring System
- Enhanced precision: The latest guidelines emphasize more detailed observations to better reflect the severity of neurological deficits.
- New symptom categories: Some symptoms have been reclassified or refined, improving the clarity of diagnosis.
- Updated thresholds: Adjustments in scoring thresholds aim to minimize misinterpretations and ensure timely interventions.
How to Prepare for Accurate Evaluation
Preparation is vital for achieving consistent results when using these diagnostic tools. Professionals must stay up to date with the latest guidelines and ensure that their assessment techniques are aligned with the most current standards. This includes regular practice, reviewing patient history, and understanding the latest symptom categories and scoring methods.
Steps for Effective Assessment
- Review patient history and symptoms thoroughly.
- Familiarize yourself with the most recent scoring updates.
- Ensure consistent evaluation practices across all team members.
Why Precision Matters
Accurate results not only affect immediate treatment decisions but also influence long-term rehabilitation and recovery. Proper application of these evaluation methods leads to a better understanding of brain function, ultimately improving patient care and recovery outcomes. Missteps in the evaluation process can delay intervention and hinder the overall treatment plan.
In conclusion, mastering these diagnostic tools is essential for all healthcare professionals involved in stroke management. The ongoing updates ensure that the tools remain effective and applicable to the evolving needs of patients.
Overview of Stroke Assessment 2025
Key Updates in Evaluation 2025
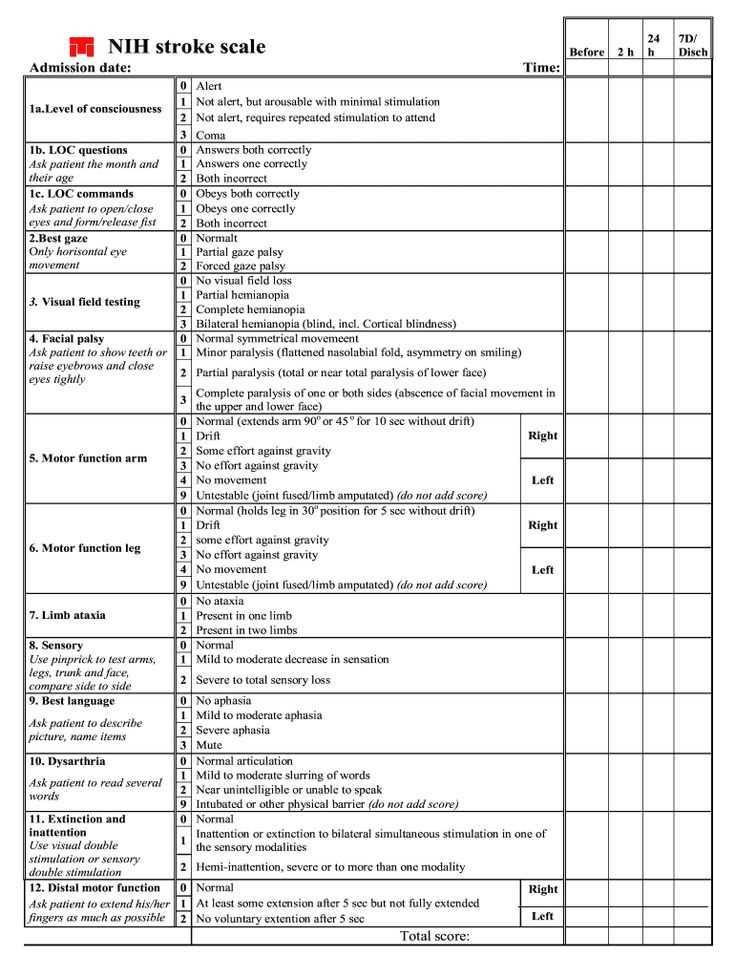
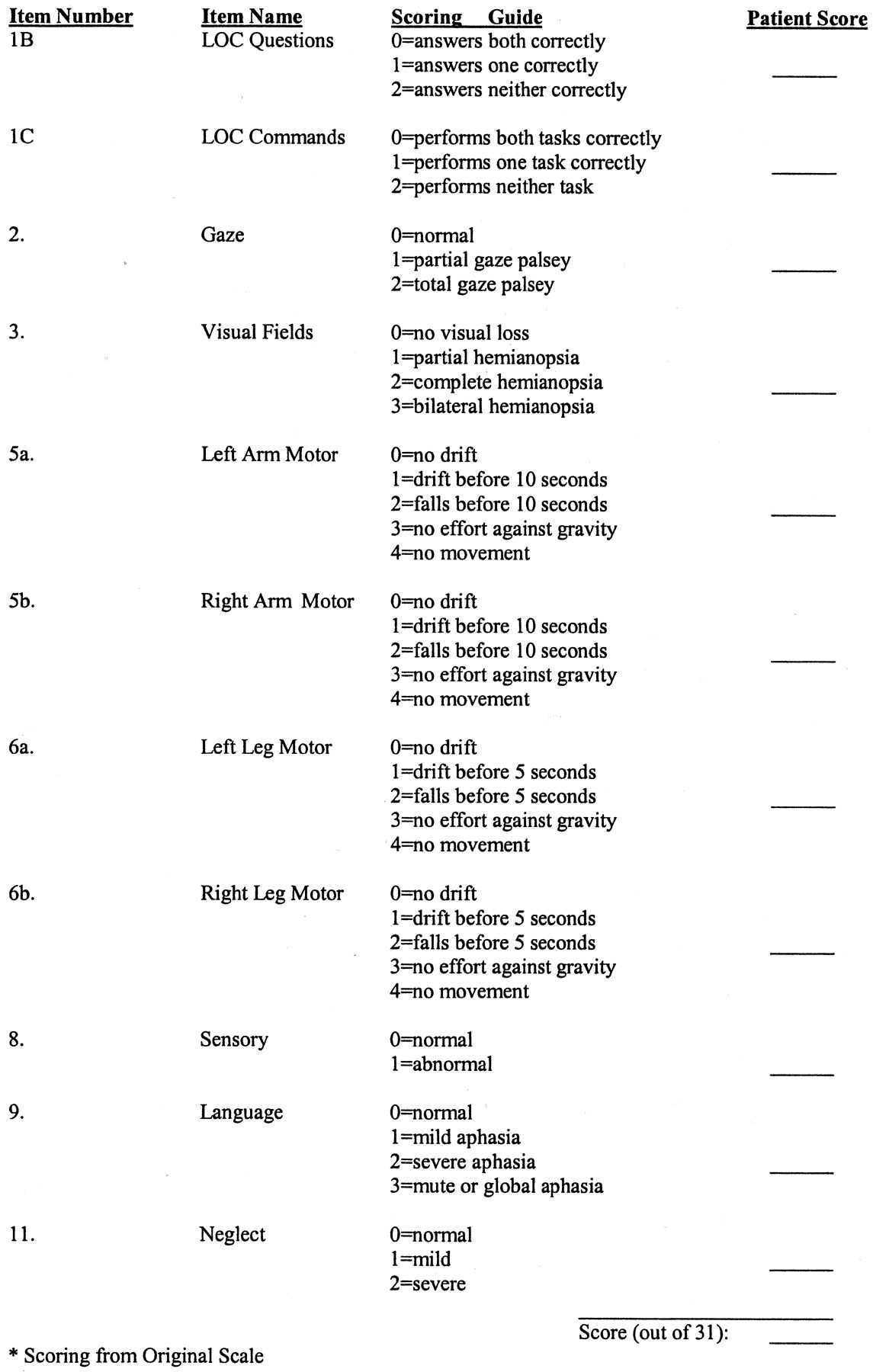
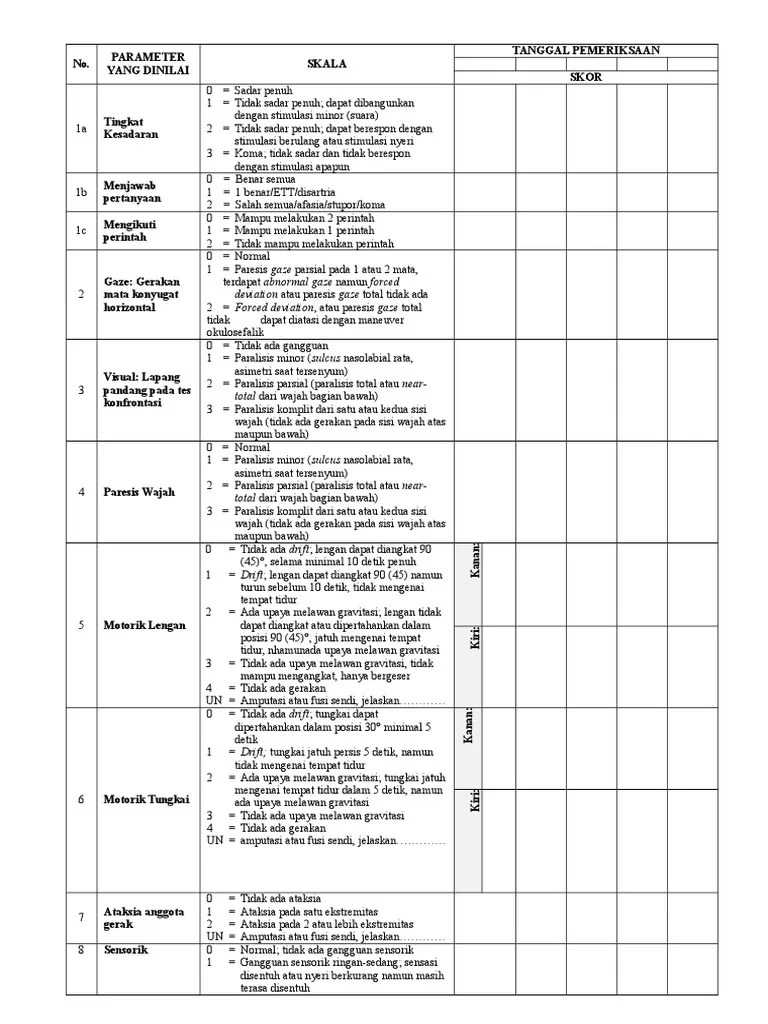
Understanding the Scoring System
How to Prepare for the Evaluation
Common Pitfalls in Stroke Assessment
Why Accuracy is Crucial in 2025
Effective evaluation of neurological impairments is critical for accurate diagnosis and treatment planning. This section explores the key components of the current stroke assessment system, focusing on the latest modifications and the overall approach to scoring. The importance of thorough preparation and avoiding common errors is also discussed to ensure reliable results in clinical settings.
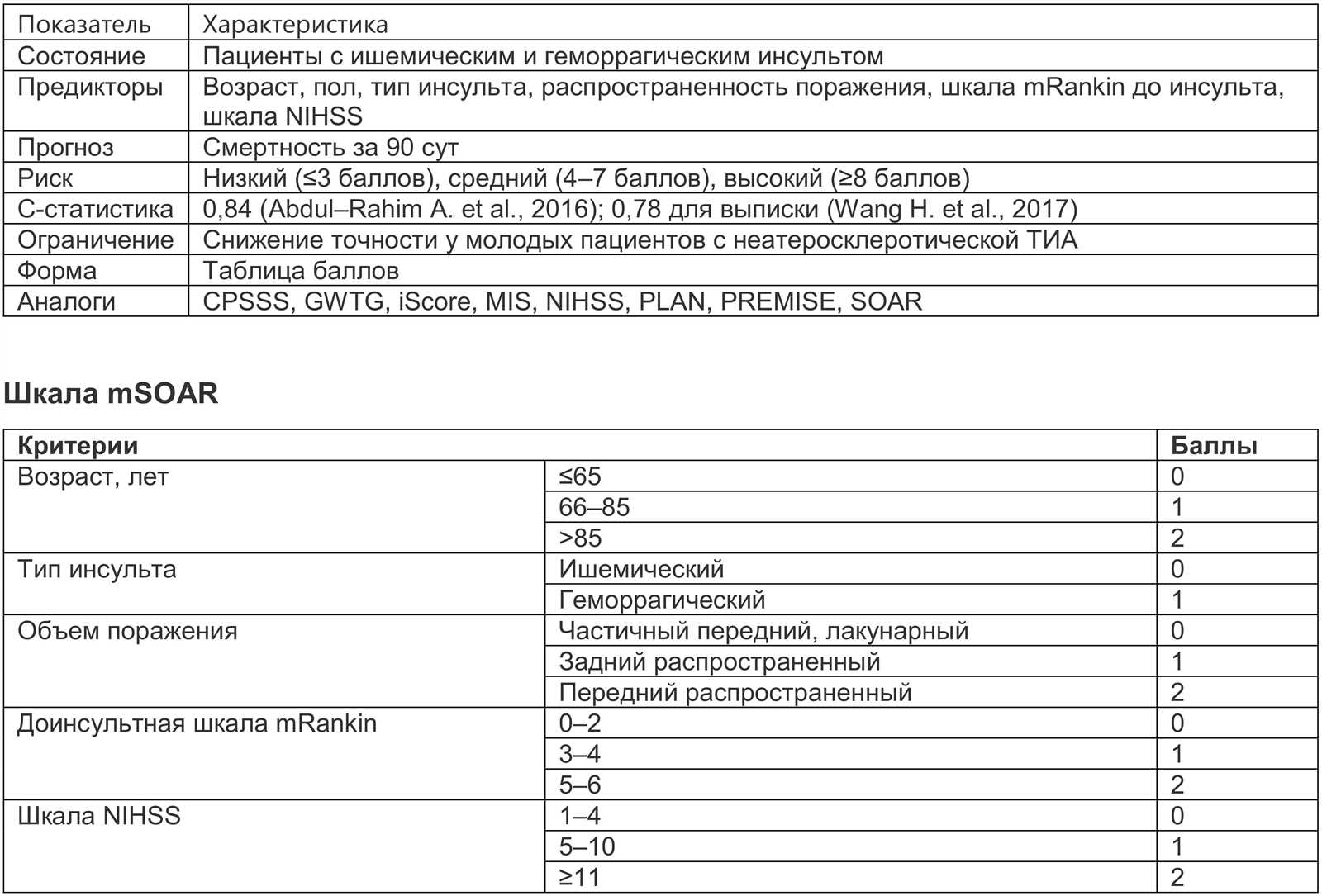
Significant updates have been made to the assessment criteria, with a focus on improving precision and reflecting the latest research. These changes aim to provide a more detailed understanding of a patient’s condition, enhancing the decision-making process for healthcare providers. The scoring system has been refined to better capture the severity of neurological deficits, ensuring that every patient receives the appropriate level of care.
Understanding the structure of the evaluation process is crucial for accurate interpretation. The scoring system is designed to reflect various aspects of neurological function, from motor skills to speech and cognition. Familiarity with each component allows clinicians to assess the patient’s condition thoroughly and make informed decisions about their treatment.
Preparation plays a vital role in achieving accurate results. Professionals must stay informed about the most recent changes to the assessment criteria and practice using the system regularly. This ensures consistency in evaluations and helps identify any potential issues early on. Additionally, reviewing past cases and staying current with research can improve diagnostic skills and enhance patient care.
One of the most common mistakes in the evaluation process is misinterpreting the symptoms or applying the wrong scoring thresholds. These errors can lead to incorrect diagnoses and delays in treatment. It’s essential to be aware of subtle differences in patient presentation and carefully apply the scoring criteria to avoid these pitfalls.
Correct evaluation is essential not only for immediate treatment decisions but also for long-term outcomes. Accurate results help tailor rehabilitation plans and ensure that patients receive the most effective care. In 2025, the precision of assessments is more important than ever, as new treatment options and recovery strategies rely on detailed and accurate clinical data.