Understanding the intricate relationship between parathyroid hormone (PTH), osteoporosis, and calcium homeostasis is crucial for comprehending the pathophysiology of bone disorders. PTH is a hormone secreted by the parathyroid glands, responsible for regulating calcium levels in the body. It plays a vital role in bone health, specifically in maintaining bone density and preventing conditions like osteoporosis.
Osteoporosis is a condition characterized by the loss of bone mass and weakened bone structure, leading to an increased risk of fractures. PTH and calcium homeostasis are intricately connected to this condition, as PTH stimulates the release of calcium from the bones into the bloodstream. This mechanism helps maintain normal blood calcium levels but can also lead to excessive bone resorption and the development of osteoporosis over time.
The worksheet answers related to PTH, osteoporosis, and calcium homeostasis shed light on the physiological processes underlying bone health. Understanding these answers helps comprehend the importance of PTH in maintaining the delicate balance of calcium levels in the body and the potential consequences of its dysregulation, such as osteoporosis. It also underscores the significance of proper nutrition, exercise, and medical interventions in preventing and managing bone-related disorders.
Understanding PTH (Parathyroid hormone) and its role in calcium homeostasis
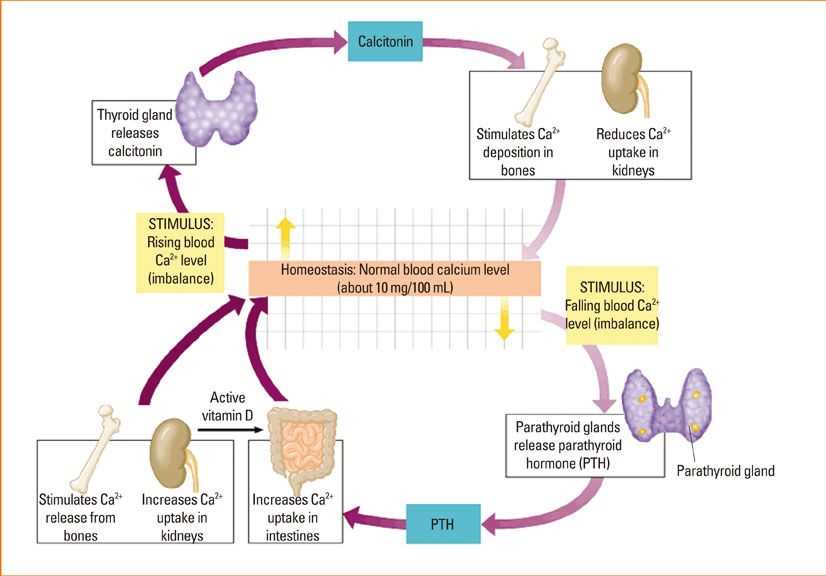
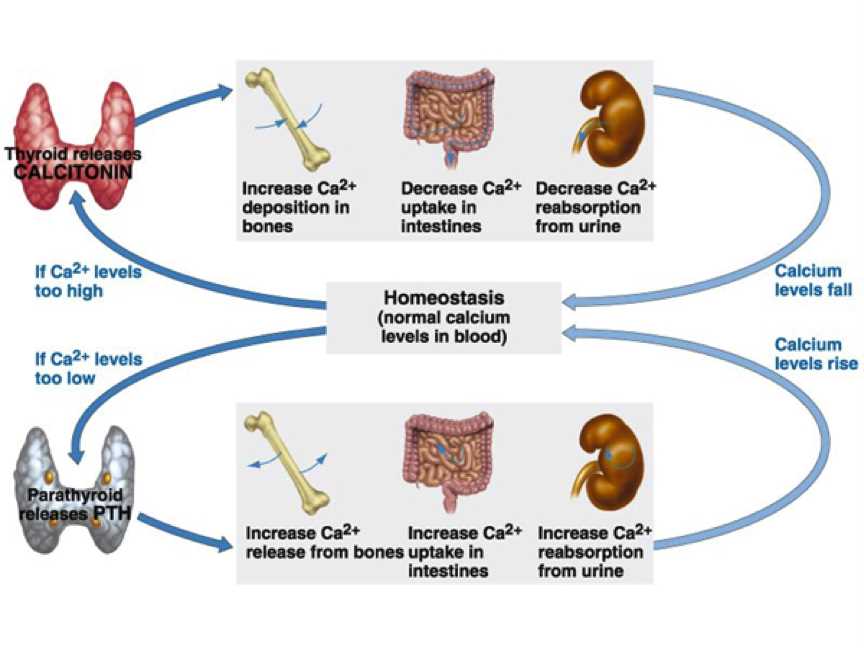
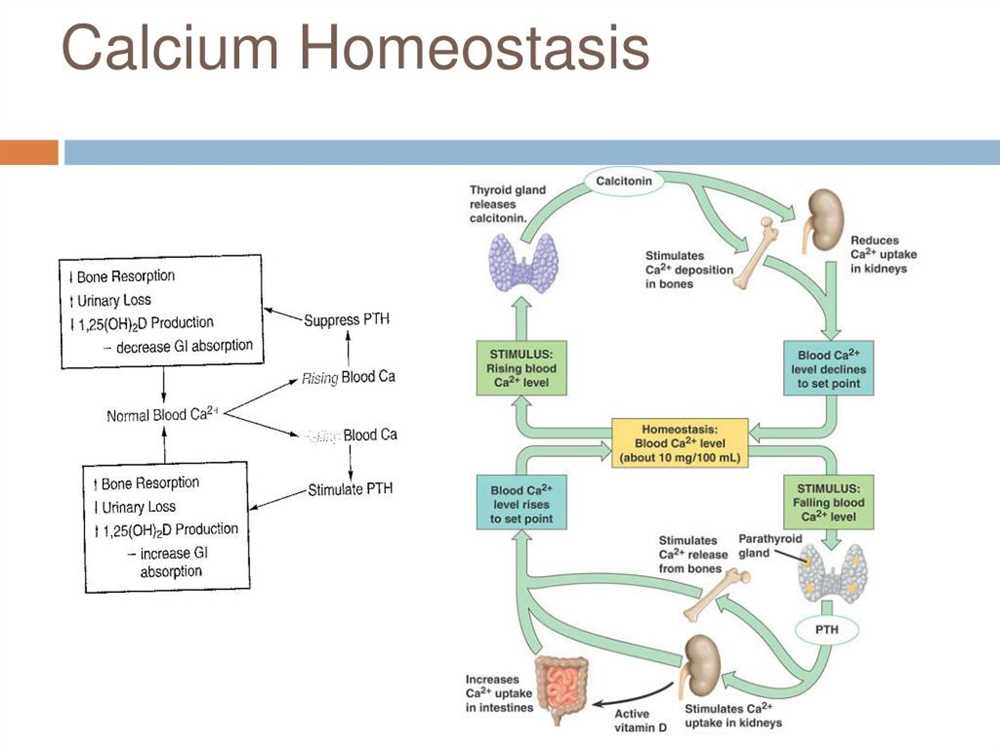
Calcium is an essential mineral that plays a crucial role in various physiological processes in the human body. It is not only responsible for maintaining the structural integrity of bones and teeth but also participates in muscle contraction, nerve conduction, blood clotting, and hormone secretion. To ensure optimal calcium levels in the blood, the body relies on a delicate balance between calcium absorption from the intestines, calcium reabsorption from the kidneys, and calcium release from the bones.
Parathyroid hormone (PTH) is a key regulator of calcium homeostasis in the body. It is produced by the parathyroid glands, which are small endocrine glands located in the neck. PTH acts on the bones, intestines, and kidneys to elevate blood calcium levels when they fall below the normal range. The primary function of PTH is to stimulate the release of calcium from the bones. When blood calcium levels are low, PTH promotes the breakdown of bone tissue and enhances the release of calcium, thus increasing blood calcium levels.
PTH also acts on the kidneys to promote the reabsorption of calcium from the urine, preventing its excretion. This process helps to conserve calcium and maintain adequate levels in the blood. In addition, PTH enhances the production of calcitriol, the active form of vitamin D, which plays a vital role in calcium absorption from the intestines. Calcitriol acts in conjunction with PTH to increase intestinal calcium absorption, ensuring that sufficient calcium is absorbed into the bloodstream.
In summary, PTH plays a critical role in calcium homeostasis by stimulating calcium release from the bones, promoting renal calcium reabsorption, and enhancing intestinal calcium absorption. By maintaining optimal blood calcium levels, PTH ensures the proper functioning of various physiological processes. Imbalances in PTH levels can lead to disorders such as hyperparathyroidism or hypoparathyroidism, which can have profound effects on calcium homeostasis and overall health.
Effects of PTH on bones and osteoporosis development
The parathyroid hormone (PTH) plays a crucial role in the maintenance of calcium homeostasis in the body. PTH primarily acts on the bones and kidneys to regulate calcium levels in the blood. However, excessive or prolonged PTH secretion can lead to adverse effects on bone health and contribute to the development of osteoporosis.
One of the main effects of PTH on bones is the stimulation of bone resorption. PTH activates osteoclasts, the cells responsible for breaking down bone tissue, leading to the release of calcium into the bloodstream. This resorption process helps maintain adequate calcium levels but can also result in bone loss if PTH levels are consistently elevated. Over time, increased bone resorption can weaken the bones and increase the risk of fractures.
Additionally, PTH affects bone formation. While it promotes bone resorption, it also indirectly stimulates bone formation by interacting with other cells and factors in the bone remodeling process. However, chronic elevation of PTH levels can disrupt the balance between bone resorption and formation, ultimately leading to a net loss of bone mass.
In the context of osteoporosis, the effects of PTH on bone become particularly significant. Osteoporosis is a condition characterized by low bone mass and structural deterioration of bone tissue, leading to increased fragility and susceptibility to fractures. Excessive PTH levels can accelerate bone loss and contribute to the progression of osteoporosis. Therefore, understanding the regulation of PTH and its effects on bone is crucial for developing strategies to prevent and manage osteoporosis.
References:
- Drake, M. T., & Clarke, B. L. (2018). Lewiecki EM. Pathophysiology of Osteoporosis. Clinical cases in mineral and bone metabolism: the official journal of the Italian Society of Osteoporosis, Mineral Metabolism, and Skeletal Diseases, 15(3), 164–174.
- Silva, B. C., Bilezikian, J. P., & Cusano, N. E. (2018). Primary Hyperparathyroidism. Annals of internal medicine, 168(12), ITC81–ITC96.
Exploring the relationship between PTH and calcium levels in the body
Parathyroid hormone (PTH) plays a crucial role in regulating calcium levels in the body. Calcium is essential for various physiological processes, including muscle contraction, nerve signaling, and bone formation. To maintain calcium homeostasis, the body tightly controls the levels of PTH.
When blood calcium levels drop below the normal range, special cells in the parathyroid glands detect the decrease and release PTH into the bloodstream. PTH acts on target organs, such as the bones and kidneys, to increase calcium levels. One of the key actions of PTH is the stimulation of bone resorption by osteoclasts, leading to the release of calcium from the bones into the bloodstream. Additionally, PTH promotes the reabsorption of calcium in the kidneys, preventing excessive loss of calcium through urine.
On the other hand, if blood calcium levels rise above the normal range, the parathyroid glands reduce the release of PTH, allowing the body to decrease calcium levels. This is achieved through the inhibition of bone resorption and increased calcium excretion in urine. Furthermore, PTH stimulates the production of calcitriol, the active form of vitamin D, which enhances intestinal calcium absorption and further helps to maintain calcium balance.
In summary, PTH and calcium levels in the body are intricately linked. PTH acts as a regulator, increasing calcium levels when they are too low and decreasing them when they are too high. This dynamic relationship ensures the proper functioning of various physiological processes that rely on calcium, ultimately maintaining calcium homeostasis in the body.
Mechanisms of PTH regulation and its impact on calcium balance
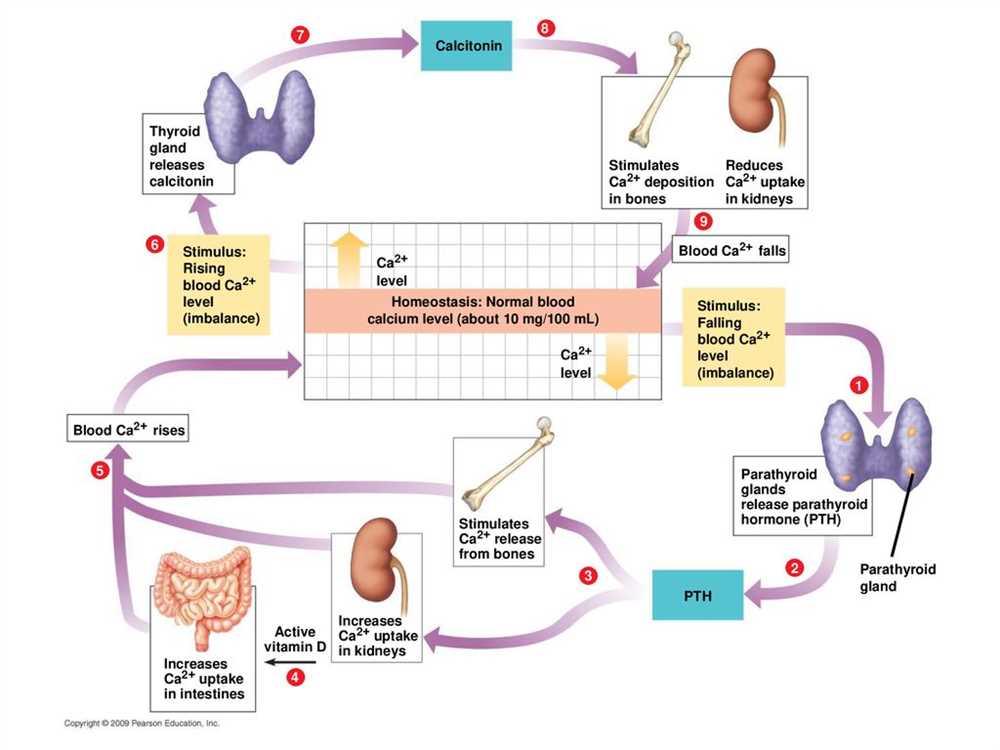
The parathyroid hormone (PTH) plays a crucial role in regulating calcium balance in the body. It is primarily produced and secreted by the parathyroid glands, which are located in the neck. PTH is released in response to low calcium levels in the blood, and its main function is to increase calcium levels by regulating its absorption, reabsorption, and excretion.
PTH acts on different target organs to achieve its calcium-balancing effects. One of the primary targets of PTH is the bones. When blood calcium levels are low, PTH stimulates bone resorption, which involves the breakdown of bone tissue and the release of calcium into the bloodstream. This mechanism helps to increase calcium levels in the blood. However, chronic excessive PTH secretion can lead to osteoporosis, a condition characterized by weak and brittle bones.
Another target of PTH is the kidneys. PTH enhances the reabsorption of calcium in the kidneys, preventing its loss in the urine and promoting its return to the bloodstream. Additionally, PTH stimulates the production of an active form of vitamin D in the kidneys, which is essential for calcium absorption from the intestines. This further aids in increasing calcium levels in the body.
Overall, the regulation of PTH and its impact on calcium balance is a highly complex process. It involves a delicate interplay between the parathyroid glands, bones, kidneys, and the intestines. Imbalances in this system can lead to disorders such as hyperparathyroidism, hypoparathyroidism, and osteoporosis. Understanding the mechanisms of PTH regulation is crucial for maintaining proper calcium homeostasis and preventing these conditions.
PTH osteoporosis and the importance of maintaining calcium homeostasis
The parathyroid hormone (PTH) plays a crucial role in maintaining calcium homeostasis in the body. PTH is secreted by the parathyroid glands, which are located in the neck. Its main function is to regulate the levels of calcium and phosphorus in the blood. PTH acts on different organs and tissues to increase calcium levels and maintain the balance required for proper bone health.
Osteoporosis is a condition characterized by weak and brittle bones. It occurs when the body loses too much calcium, leading to a decrease in bone density. PTH is directly involved in bone remodeling and helps to prevent osteoporosis. When calcium levels are low, PTH stimulates the release of calcium from the bones into the bloodstream. This allows the body to maintain normal calcium levels in the blood but can lead to decreased bone mass over time.
To maintain calcium homeostasis, it is important to have a balanced diet that includes sufficient amounts of calcium and vitamin D. Calcium-rich foods include dairy products, leafy greens, and fortified foods. Vitamin D helps the body absorb calcium from the diet. Regular exercise, especially weight-bearing exercises like walking or weightlifting, also promotes bone health and can help prevent osteoporosis.
- In conclusion, PTH plays a crucial role in maintaining calcium homeostasis and preventing osteoporosis. Its actions on the bones and other organs ensure that the body has enough calcium for various functions while maintaining bone density. Maintaining a balanced diet and engaging in regular exercise are essential for maintaining proper calcium levels and bone health.
Diagnostic tests and tools for assessing PTH levels and bone health
When it comes to assessing parathyroid hormone (PTH) levels and overall bone health, there are several diagnostic tests and tools that can be used. These tests help healthcare professionals evaluate the functioning of the parathyroid glands, which play a crucial role in calcium homeostasis and bone metabolism.
One common diagnostic test is the measurement of serum PTH levels. This is typically done through a blood test, where a sample of blood is taken and analyzed for its PTH concentration. Elevated PTH levels may indicate an overactive parathyroid gland, while low PTH levels may suggest an underactive gland. This test provides valuable information about the overall functioning of the parathyroid glands and can help identify abnormalities in calcium regulation.
In addition to PTH level measurement, there are other diagnostic tools that can assess bone health. Dual-energy X-ray absorptiometry (DXA) is a widely used technique for evaluating bone mineral density (BMD). This non-invasive test measures the density of minerals, such as calcium, in specific areas of the body, typically the spine and hips. DXA scans can help identify osteoporosis and determine the risk of fractures. The results are often expressed as a T-score, which compares an individual’s BMD to that of a young healthy adult.
Another tool for assessing bone health is a bone turnover marker test. This test measures specific biochemical markers in the blood or urine that are indicative of bone remodeling activity. Elevated levels of these markers may suggest increased bone resorption and decreased bone formation, which can be associated with conditions like osteoporosis. Examples of bone turnover markers include serum collagen type I cross-linked C-telopeptide and osteocalcin.
In conclusion, a combination of tests and tools is used to assess PTH levels and bone health. Serum PTH level measurement helps evaluate the function of the parathyroid glands, while DXA scans and bone turnover marker tests provide valuable information about bone density and remodeling activity. These diagnostic tests and tools play a crucial role in the diagnosis and management of conditions related to PTH and calcium homeostasis, such as osteoporosis.
Treatment options for PTH-related osteoporosis and calcium imbalances
Paternary hyperparathyroidism (PTH) is a condition characterized by overactive parathyroid glands that produce excessive amounts of parathyroid hormone (PTH). This can lead to imbalances in calcium levels in the body, resulting in conditions such as hypercalcemia and osteoporosis. Fortunately, there are several treatment options available to manage PTH-related osteoporosis and calcium imbalances.
One of the primary treatment approaches for PTH-related osteoporosis is the use of bisphosphonates. Bisphosphonates are medications that can help to regulate bone turnover and increase bone mineral density. They work by inhibiting the activity of osteoclasts, which are cells that break down bone tissue. By reducing bone resorption, bisphosphonates can help prevent further loss of bone mass and improve bone strength in individuals with PTH-related osteoporosis.
In addition to bisphosphonates, calcimimetics are another treatment option for PTH-related osteoporosis and calcium imbalances. Calcimimetics are drugs that mimic the action of calcium on the parathyroid glands, resulting in a decrease in PTH levels. By reducing PTH levels, calcimimetics can help to restore calcium homeostasis in individuals with PTH-related osteoporosis. This can lead to improvements in bone health and a decrease in the risk of fractures.
Other treatment options for individuals with PTH-related osteoporosis and calcium imbalances include hormone replacement therapy (such as estrogen or testosterone), vitamin D supplementation, and dietary changes. Hormone replacement therapy can help to regulate hormone levels and promote bone health. Vitamin D supplementation is important for individuals with PTH-related calcium imbalances because it aids in the absorption of calcium from the intestines and helps maintain proper calcium levels in the blood. Dietary changes, such as increasing calcium intake through foods or supplements, can also be beneficial in managing PTH-related osteoporosis and calcium imbalances.
In summary, treatment options for PTH-related osteoporosis and calcium imbalances include bisphosphonates, calcimimetics, hormone replacement therapy, vitamin D supplementation, and dietary changes. These treatments aim to regulate PTH levels, improve calcium balance, and promote bone health. It is important for individuals with PTH-related osteoporosis to work closely with their healthcare provider to determine the most appropriate treatment plan for their specific condition.