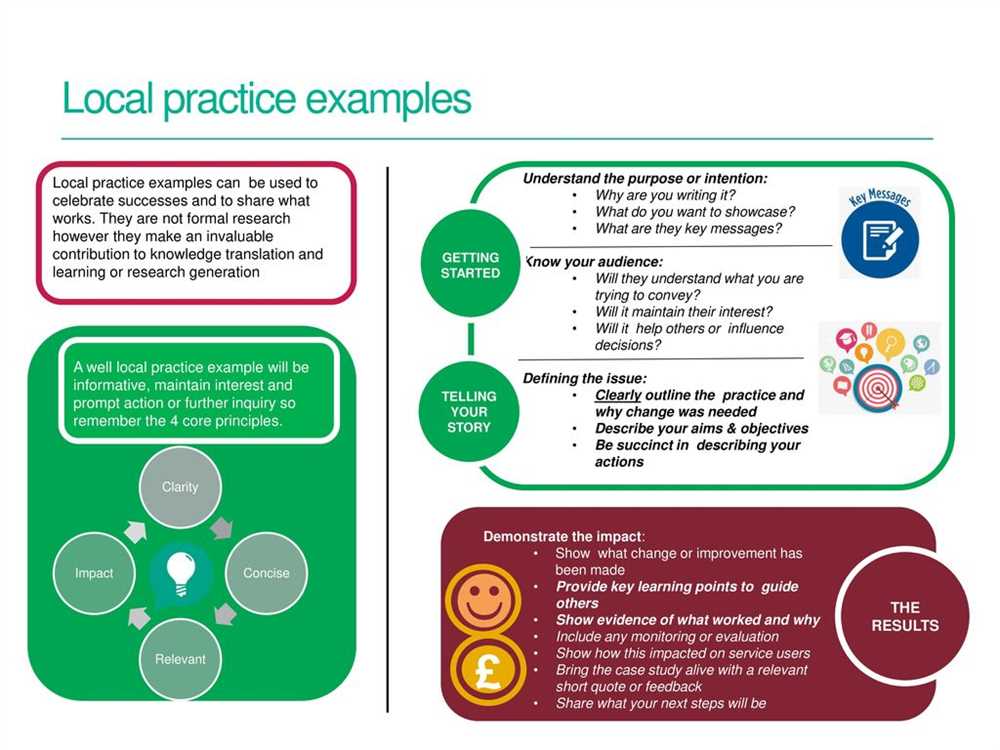
Health information management (HIM) plays a crucial role in the effective and efficient management of healthcare data. This is where case studies come in – they provide real-world examples that demonstrate the various challenges and solutions in HIM. By analyzing and understanding these case studies, healthcare professionals can gain valuable insights into best practices and strategies for managing health information.
One key aspect of HIM is data quality and integrity. Case studies can shed light on how organizations address issues such as incomplete or inaccurate patient records, duplicate records, or outdated information. These case studies often highlight the importance of regular data audits, staff training, and the implementation of standardized processes to ensure data accuracy.
Another important area that case studies can cover is information privacy and security. With the increasing use of electronic health records, protecting sensitive patient information has become a top priority. Case studies can explore the measures organizations take to safeguard personal health information, such as implementing encryption protocols, access controls, and regular security assessments.
Furthermore, case studies can also delve into the role of health information management in improving patient care and outcomes. This may include examples of how HIM professionals collaborate with healthcare providers to ensure prompt and accurate diagnosis, treatment, and follow-up care. These case studies can highlight the use of health information exchange systems, decision support tools, and data analytics to optimize patient care delivery.
In conclusion, health information management case studies provide a valuable resource for understanding the complexities of managing healthcare data. They offer insights into data quality, privacy and security, as well as the role of HIM in improving patient care. By examining these case studies and their answer key, healthcare professionals can stay informed about best practices and innovation in health information management.
Health Information Management Case Studies Answer Key

In the field of health information management, case studies are often used to provide practical examples and real-world scenarios for students and professionals to analyze and learn from. These case studies typically present a specific healthcare situation or problem, and require the application of knowledge and critical thinking skills to find solutions or make recommendations. This answer key serves as a guide to help individuals understand and interpret the case study questions, as well as provide suggested answers or approaches.
Case Study 1: Electronic Health Record Implementation
- Question 1: What are the key steps involved in implementing an electronic health record (EHR) system?
- Answer: The key steps in implementing an EHR system include strategic planning, system selection, system design and customization, data migration, staff training, system testing and validation, and system go-live and post-implementation support.
- Question 2: What challenges might arise during the EHR implementation process?
- Answer: Some challenges that might arise during the EHR implementation process include resistance to change from healthcare professionals, interoperability issues between different systems, data integrity and accuracy concerns, and financial and resource constraints.
- Question 3: What are the potential benefits of implementing an EHR system?
- Answer: Some potential benefits of implementing an EHR system include improved patient care coordination, increased efficiency in healthcare workflows, reduced medical errors, enhanced data accessibility and sharing, and the ability to generate data-driven insights for decision-making.
Case Study 2: Health Information Exchange (HIE) Implementation
- Question 1: What is the purpose of a Health Information Exchange (HIE) system?
- Answer: The purpose of an HIE system is to facilitate the secure and electronic exchange of patient health information between healthcare organizations, enabling timely access to complete and accurate patient records across different care settings.
- Question 2: What are the potential benefits and challenges of implementing an HIE system?
- Answer: Some potential benefits of implementing an HIE system include improved care coordination, reduced duplicate tests and treatments, enhanced patient safety, and increased efficiency in healthcare delivery. However, challenges such as data privacy and security concerns, interoperability issues, and resistance to sharing information among healthcare providers may arise.
- Question 3: What strategies can be employed to overcome the challenges of HIE implementation?
- Answer: Strategies to overcome HIE implementation challenges include establishing and enforcing robust data privacy and security measures, promoting standardized data formats and protocols for interoperability, addressing legal and policy barriers, and educating healthcare professionals about the benefits of information sharing.
By using this answer key, individuals can gain a deeper understanding of the case study scenarios and the key concepts and considerations involved in health information management. It serves as a valuable resource for learning and applying healthcare informatics principles in real-world situations.
Case Study 1: Enhancing Patient Care with Electronic Health Records
In this case study, we examine how the implementation of electronic health records (EHRs) has enhanced patient care at a fictional healthcare organization.
Background:
The healthcare organization in question had been using paper-based medical records for many years, which proved to be inefficient and time-consuming. The staff found it difficult to access patient information quickly, resulting in delays in providing appropriate care. Therefore, the organization decided to transition to EHRs to streamline their processes and improve patient care.
Implementation:
The transition to EHRs began with a comprehensive training program for all staff members. They were taught how to use the new electronic system and how to input patient data accurately. Additionally, the organization invested in new hardware and software to support the implementation. The EHR system was designed to integrate with existing healthcare systems, such as laboratory and pharmacy systems, to ensure seamless information flow.
Benefits:
The implementation of EHRs resulted in several benefits for the healthcare organization and its patients. Firstly, the electronic system allowed for easy access to patient information, eliminating the need to search through paper records. This significantly improved workflow efficiency, as healthcare providers could quickly retrieve and review patient data, leading to faster diagnosis and treatment.
Furthermore, the electronic system facilitated better communication among healthcare providers. Different departments and professionals could easily share patient information and coordinate care, resulting in a more holistic approach to treatment. Additionally, the EHR system provided decision support tools, such as reminders and alerts, to help healthcare providers make informed decisions and improve patient outcomes.
Conclusion:
The implementation of electronic health records has transformed the healthcare organization’s ability to provide quality care to their patients. The transition from paper-based records to EHRs has streamlined processes, improved workflow efficiency, and enhanced communication among healthcare providers. Ultimately, this has resulted in faster diagnosis and treatment, as well as improved patient outcomes.
Case Study 2: Managing Health Data Privacy and Security
In this case study, we examine the challenges of managing health data privacy and security within a healthcare organization. The case study focuses on the implementation of a new electronic health record (EHR) system and the potential risks that come with storing and managing sensitive patient information.
Background: The healthcare organization, a large hospital, recently transitioned from paper-based medical records to an EHR system. The new system allows healthcare providers to access and share patient information more efficiently. However, this transition has raised concerns about the privacy and security of sensitive health data.
Challenges: One of the main challenges faced by the organization is ensuring the privacy of patient information. With the transition to an electronic system, there is an increased risk of unauthorized access to patient data. The organization needs to implement robust security measures, such as user authentication and encryption, to prevent unauthorized individuals from accessing sensitive health information.
Solutions: To address the privacy and security challenges, the organization can implement several strategies. First, they can train staff members on the importance of data privacy and security and provide guidelines on how to handle patient information securely. Additionally, the organization should regularly update and patch their EHR system to address any potential vulnerabilities. Data encryption and access controls should also be implemented, ensuring that only authorized individuals have access to sensitive patient information.
- One of the key solutions is to conduct regular security audits and risk assessments to identify any potential vulnerabilities in the system and address them promptly.
- The organization should also have a comprehensive data breach response plan in place to mitigate the impact of any potential security incidents.
- Regular staff training and education programs should be conducted to ensure that employees are aware of the latest privacy and security protocols.
- The organization should also establish a strong partnership with IT experts and vendors to receive ongoing support and guidance on managing data privacy and security.
Conclusion: Managing health data privacy and security is crucial in the era of electronic health records. The case study highlights the challenges faced by healthcare organizations in ensuring the privacy and security of patient information. By implementing robust security measures, conducting regular audits, and providing staff training, organizations can mitigate the risks associated with managing health data and protect patient confidentiality.
Case Study 3: Improving Coding Accuracy and Reimbursement
In this case study, we will explore how a healthcare organization was able to improve its coding accuracy and reimbursement through the implementation of a new health information management system.
The healthcare organization in question was faced with numerous challenges related to coding accuracy and reimbursement. The existing system was outdated and inefficient, leading to coding errors and subsequent denials of reimbursement claims. This resulted in financial losses for the organization and increased administrative burden.
To address these challenges, the organization decided to implement a new health information management system that would automate and streamline the coding process. The new system utilized advanced algorithms and machine learning to ensure accurate and efficient coding.
The implementation of the new system resulted in significant improvements in coding accuracy and reimbursement. The automated coding process eliminated human errors and reduced the number of coding discrepancies. As a result, the organization experienced a decrease in denied reimbursement claims and an increase in overall revenue.
The new system also allowed for better monitoring and auditing of the coding process. This helped identify any potential issues or discrepancies at an early stage, allowing for prompt resolution. Additionally, the system provided real-time feedback to coding staff, enabling them to address any coding errors immediately.
In conclusion, the implementation of a new health information management system proved to be instrumental in improving coding accuracy and reimbursement for the healthcare organization in this case study. Through automation, advanced algorithms, and real-time feedback, the organization was able to reduce coding errors, minimize denials, and increase revenue. This case study demonstrates the importance of leveraging technology in healthcare organizations to optimize coding processes and improve financial outcomes.
Case Study 4: Implementing Health Information Exchange

The implementation of health information exchange (HIE) can greatly improve the efficiency and effectiveness of healthcare services, allowing for the secure sharing of patient information across different healthcare providers. This case study focuses on the successful implementation of HIE in a large hospital system.
Background: The hospital system consists of multiple hospitals and clinics spread across a wide geographic area. The lack of interoperability between their electronic health record (EHR) systems posed a significant challenge in sharing patient information seamlessly. This resulted in delays in accessing critical patient data, duplication of tests, and potential errors in diagnoses and treatment plans.
Key Challenges:
- Lack of standardized data exchange protocols
- Incompatibility between different EHR systems
- Data security and privacy concerns
- Resistance to change from healthcare providers
Solution:
The hospital system opted to implement a robust health information exchange platform that would address these challenges. The key components of the solution included:
- Standardization: Implementing industry-standard data exchange protocols, such as HL7 and CDA, to ensure seamless communication between different EHR systems.
- Interoperability: Building interfaces and connectors that allowed for the exchange of patient data between different EHR systems, regardless of vendor or version.
- Data security: Implementing stringent access controls, encryption, and audit trails to safeguard patient information and comply with HIPAA regulations.
- Change management: Offering comprehensive training and support to healthcare providers to ensure smooth adoption and utilization of the HIE platform.
Results:
The successful implementation of the HIE platform resulted in several positive outcomes:
- Improved care coordination: Healthcare providers could access patient information in real-time, enabling them to make more informed decisions and provide better coordinated care.
- Reduced errors and duplication: The HIE platform eliminated the need for redundant tests and procedures, reducing the risk of errors and unnecessary costs.
- Enhanced patient experience: Patients experienced smoother transitions between different healthcare providers, as their medical history and records were readily available.
- Cost savings: The hospital system achieved cost savings by reducing administrative overhead, streamlining workflows, and optimizing resource utilization.
In conclusion, the implementation of health information exchange proved to be a successful solution for this hospital system, improving the efficiency and quality of patient care while ensuring the security and privacy of sensitive health information.