Glucose and glucagon are two crucial components of our body’s metabolic system. Glucose is the primary source of energy for our cells, while glucagon is a hormone that helps regulate glucose levels in the bloodstream. The delicate balance between these two substances is necessary for maintaining overall health and proper bodily functioning.
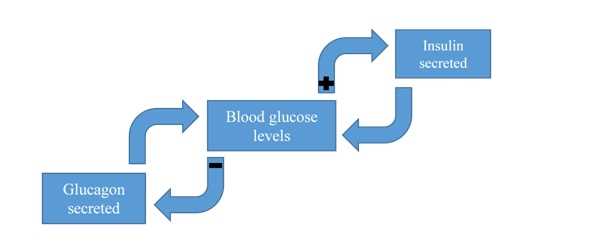
The regulation of glucose and glucagon levels is achieved through a series of feedback loops within the body. These loops ensure that glucose is available when needed and that excessive levels are controlled, thus preventing health issues such as diabetes. Understanding the intricate workings of these feedback loops provides valuable insights into how our bodies maintain homeostasis and respond to changing conditions.
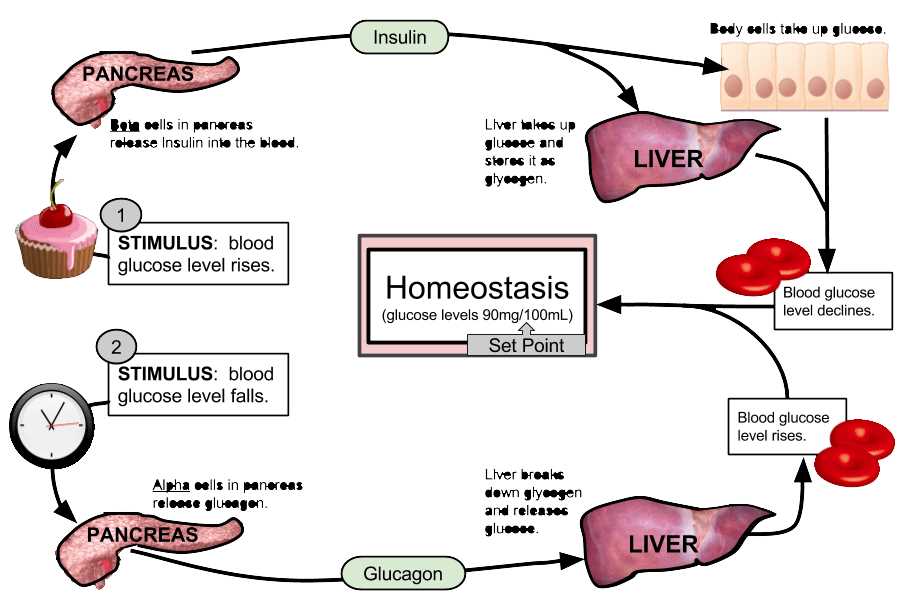
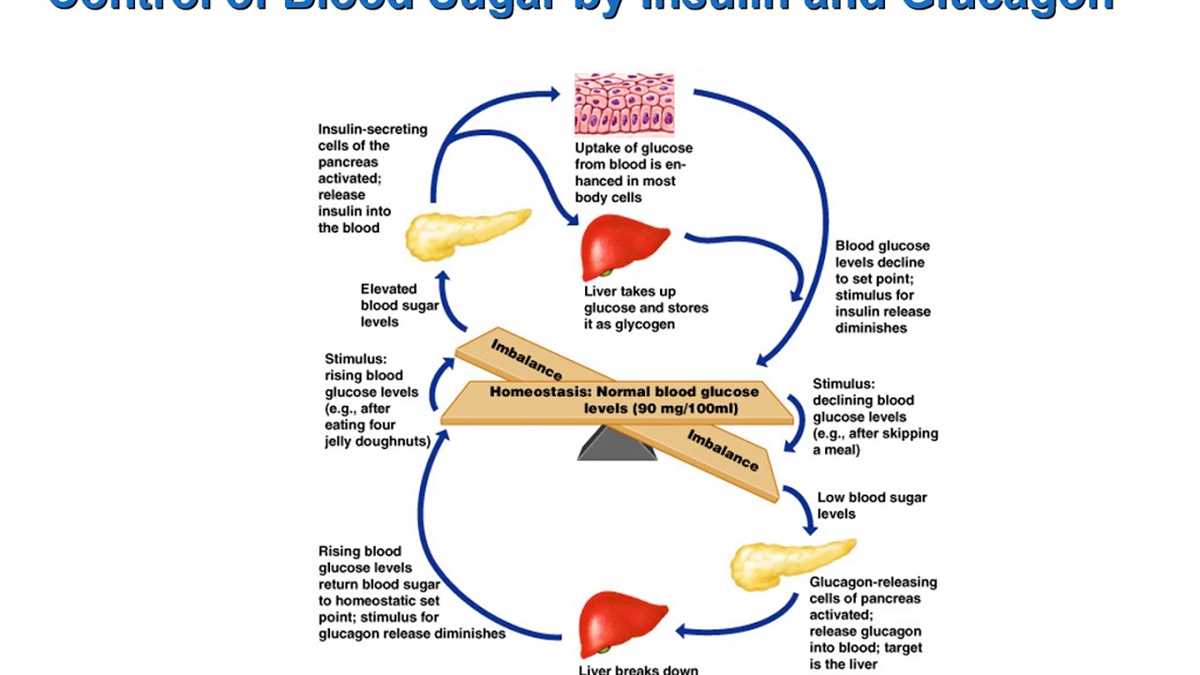
One of the key feedback loops involves the pancreatic cells. When blood glucose levels rise, specialized cells in the pancreas called beta cells detect this increase and release the hormone insulin. Insulin acts as a signal to various cells in the body, prompting them to take up glucose from the bloodstream and store it for later use. This process helps lower blood glucose levels and maintain balance. Conversely, when blood glucose levels drop, the alpha cells in the pancreas release glucagon, which signals the liver to break down stored glycogen and release glucose into the bloodstream, raising blood glucose levels.
This feedback loop between glucose, insulin, and glucagon is finely tuned to ensure that the body always has enough glucose for energy but not an excess that could lead to potential harm. The regulation of these substances is influenced by various factors, including diet, physical activity, and hormonal changes. Understanding the intricate mechanisms of this feedback loop can serve as a foundation for managing and preventing diabetes and other metabolic disorders.
Understanding glucose regulation and the role of glucagon

Glucose regulation is a crucial process in the body that ensures a stable and optimal level of glucose in the bloodstream. Glucose is the primary source of energy for cells, and its levels need to be tightly controlled. The body has a complex feedback system involving various hormones and organs to maintain glucose homeostasis.
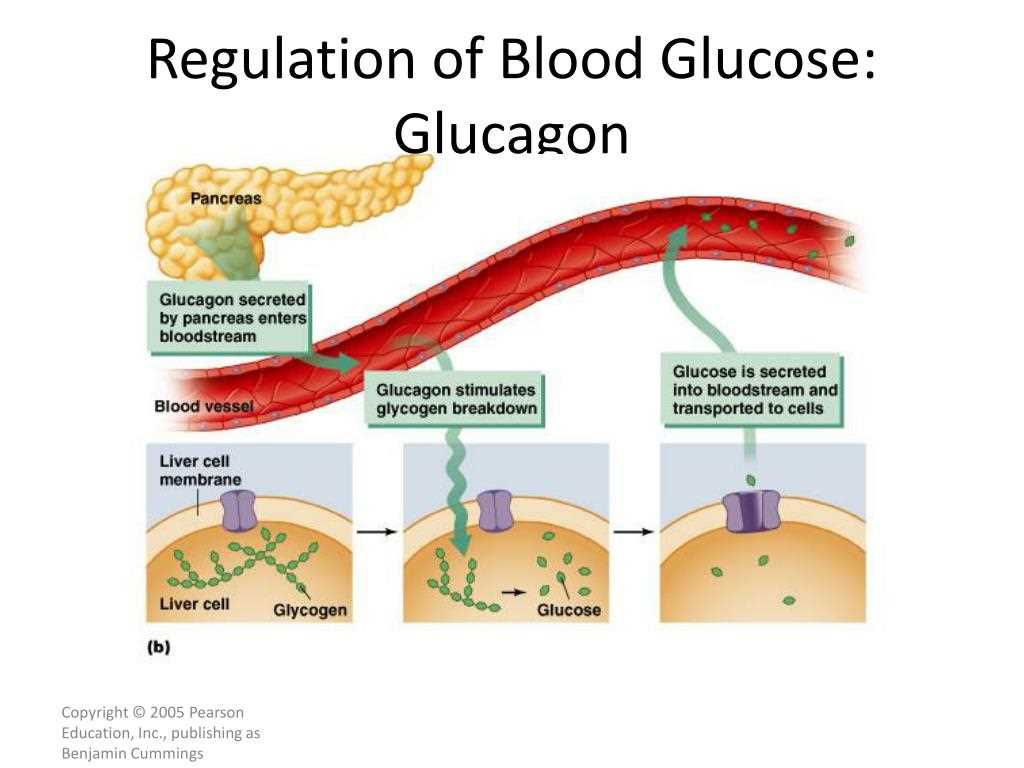
The key players in glucose regulation are insulin and glucagon, two hormones produced by the pancreas. Insulin is released when blood glucose levels are high, signaling cells to take up glucose from the bloodstream and store it. On the other hand, when blood glucose levels drop, the pancreas secretes glucagon to stimulate the liver to break down glycogen and release glucose into the bloodstream. This process helps raise blood glucose levels to ensure a consistent supply of energy to the body.
Glucagon acts by binding to specific receptors on liver cells, activating enzymes involved in glycogenolysis, the breakdown of glycogen into glucose. It also promotes gluconeogenesis, the synthesis of glucose from non-carbohydrate sources like amino acids and fatty acids. By increasing blood glucose levels, glucagon plays a crucial role in preventing hypoglycemia and providing energy during fasting or prolonged exercise.
In addition to its role in glucose regulation, glucagon also affects other metabolic processes. It stimulates lipolysis, the breakdown of fats, and ketogenesis, the production of ketone bodies. These metabolic actions help provide alternative energy sources when glucose levels are low.
To summarize, glucose regulation is a dynamic process involving a feedback loop between insulin and glucagon. Insulin acts to lower blood glucose levels by promoting glucose uptake and storage, while glucagon acts to raise blood glucose levels by stimulating glycogenolysis and gluconeogenesis. Understanding the role of glucagon in glucose regulation is essential for maintaining a healthy balance of blood glucose levels and ensuring adequate energy supply to the body.
Feedback loops in glucose and glucagon regulation
Glucose and glucagon are key players in the regulation of blood sugar levels in the body. When blood sugar levels drop, the body initiates a feedback loop to restore balance. This feedback loop involves the release of glucagon, a hormone produced by the pancreas, which helps to increase blood sugar levels.
The feedback loop begins with the detection of low blood sugar levels by specialized cells in the pancreas called alpha cells. These cells respond by releasing glucagon into the bloodstream. Once in the bloodstream, glucagon travels to the liver, where it promotes the breakdown of glycogen, a stored form of glucose, into glucose. This glucose is then released into the bloodstream, raising blood sugar levels.
As blood sugar levels rise, the body detects this increase and initiates a negative feedback loop to prevent excessive elevation. Insulin, another hormone produced by the pancreas, is released in response to high blood sugar levels. Insulin helps to lower blood sugar levels by facilitating the uptake of glucose into cells, where it can be used for energy or stored as glycogen.
This feedback loop ensures that blood sugar levels are kept within a narrow range, balancing the needs of the body for energy while preventing glucose levels from becoming too high or too low. It is an intricate system that relies on the coordinated actions of multiple hormones and organs, working together to maintain homeostasis in the body.
The Role of Insulin in Glucose Regulation
The hormone insulin plays a crucial role in the regulation of glucose in our body. It is produced by the beta cells of the pancreas and acts as a key regulator of blood sugar levels. Insulin’s main function is to facilitate the uptake of glucose by cells throughout the body, allowing them to use it as a source of energy.
When we consume carbohydrates, they are broken down into glucose, which enters the bloodstream. Elevated blood glucose levels trigger the release of insulin from the pancreas. Insulin binds to receptors on cell membranes, signaling them to open glucose transporters, particularly in muscle and fat cells. These transporters allow glucose to enter the cells, where it can be used for energy or stored as glycogen for later use.
Insulin not only promotes glucose uptake but also inhibits the production of glucose by the liver. It suppresses the release of glucagon, another pancreatic hormone, which acts to increase blood glucose levels. By inhibiting the breakdown of glycogen and glucose production, insulin helps maintain blood sugar levels within a narrow range.
Insulin also plays a pivotal role in regulating fat metabolism. It promotes the uptake of triglycerides into adipose tissue, where they are stored as fat. Additionally, insulin inhibits the breakdown of stored fats, preventing excessive release of fatty acids into the bloodstream.
Ultimately, insulin acts as a key player in maintaining glucose homeostasis. It ensures that glucose is efficiently taken up and utilized by cells, while also preventing excessive glucose production and fat breakdown. Dysfunction in insulin regulation can result in various metabolic disorders, such as diabetes mellitus, where blood sugar levels are chronically elevated.
Factors affecting glucose and glucagon feedback loops
The regulation of glucose levels in the body is a complex process involving various factors that affect the feedback loops of glucose and glucagon. One important factor is the intake of carbohydrates through the diet. When carbohydrates are digested, they are converted into glucose, which is then absorbed into the bloodstream. This triggers the release of insulin, a hormone that helps cells take up glucose and lowers blood sugar levels. On the other hand, if carbohydrate intake is low, the body may rely on other energy sources, such as stored glycogen or fatty acids, which can lead to an increase in blood sugar levels.
Another factor that affects glucose and glucagon feedback loops is physical activity. During exercise, muscles require more energy, and the body responds by increasing the release of glucagon. Glucagon stimulates the liver to break down glycogen and release glucose into the bloodstream, supplying the muscles with fuel. This helps maintain blood sugar levels during physical activity. However, intense or prolonged exercise can deplete glycogen stores, leading to a decrease in blood sugar levels.
In addition to diet and physical activity, hormones also play a crucial role in regulating glucose and glucagon feedback loops. For example, cortisol, a stress hormone, can increase blood sugar levels by stimulating the liver to release glucose. Growth hormone, produced by the pituitary gland, has the opposite effect, promoting glucose uptake and decreasing blood sugar levels. Hormonal imbalances or disorders can disrupt the feedback loops and result in abnormal blood sugar levels.
Other factors that affect glucose and glucagon feedback loops include medications, such as insulin injections or oral hypoglycemic drugs, which can regulate blood sugar levels. Certain medical conditions, such as diabetes or hormonal disorders, can also impact the feedback loops, leading to abnormal glucose regulation. Genetic factors can also influence an individual’s susceptibility to developing conditions that affect glucose and glucagon feedback loops.
In summary, glucose and glucagon feedback loops are influenced by various factors including diet, physical activity, hormones, medications, medical conditions, and genetics. Understanding and managing these factors are essential for maintaining optimal blood sugar levels and overall health.
Dysregulation and Disease Implications
Regulation of glucose and glucagon is essential for maintaining normal blood sugar levels and overall metabolic homeostasis. Dysregulation of this feedback loop can lead to various diseases and health conditions.
One major disease implication of dysregulation in the glucose and glucagon feedback loop is diabetes mellitus. In type 1 diabetes, the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. Without enough insulin, glucose cannot enter the cells and remains in the bloodstream, leading to high blood sugar levels. In type 2 diabetes, the body becomes resistant to the effects of insulin, leading to similar problems with glucose uptake.
Dysregulation of this feedback loop can also contribute to other metabolic disorders, such as metabolic syndrome and obesity. Insulin resistance and elevated blood sugar levels can lead to excessive storage of energy as fat, contributing to weight gain and obesity. Additionally, dysregulation of glucagon can disrupt the balance of glucose production and breakdown in the liver, leading to abnormal blood sugar levels.
In conclusion, the feedback loop between glucose and glucagon is a crucial mechanism for maintaining normal blood sugar levels. Dysregulation of this feedback loop can have significant implications for disease development, particularly in diabetes and metabolic disorders. Understanding the intricate balance between glucose and glucagon is essential for developing effective treatments and interventions for these conditions.