Preparing for an ATI Pharmacology Exam 1 can be an overwhelming task. With countless medications, drug classifications, and therapeutic uses to memorize, it’s important to have a solid study plan in place. This article aims to provide a comprehensive review of the key concepts and topics that are commonly tested on an ATI Pharmacology Exam 1.
One of the crucial areas to focus on when studying for an ATI Pharmacology Exam 1 is understanding the different drug classes and their respective actions. Pharmacology is all about how drugs interact with the body and how they produce therapeutic effects. From beta blockers to diuretics, understanding the mechanisms of action and nursing implications for each drug class is essential for success in the exam.
In addition to drug classes, ATI Pharmacology Exam 1 also tests students’ knowledge of medication administration and safety considerations. It’s important to be familiar with the proper techniques for medication administration, including routes of administration, dosage calculations, and the important guidelines for preventing medication errors.
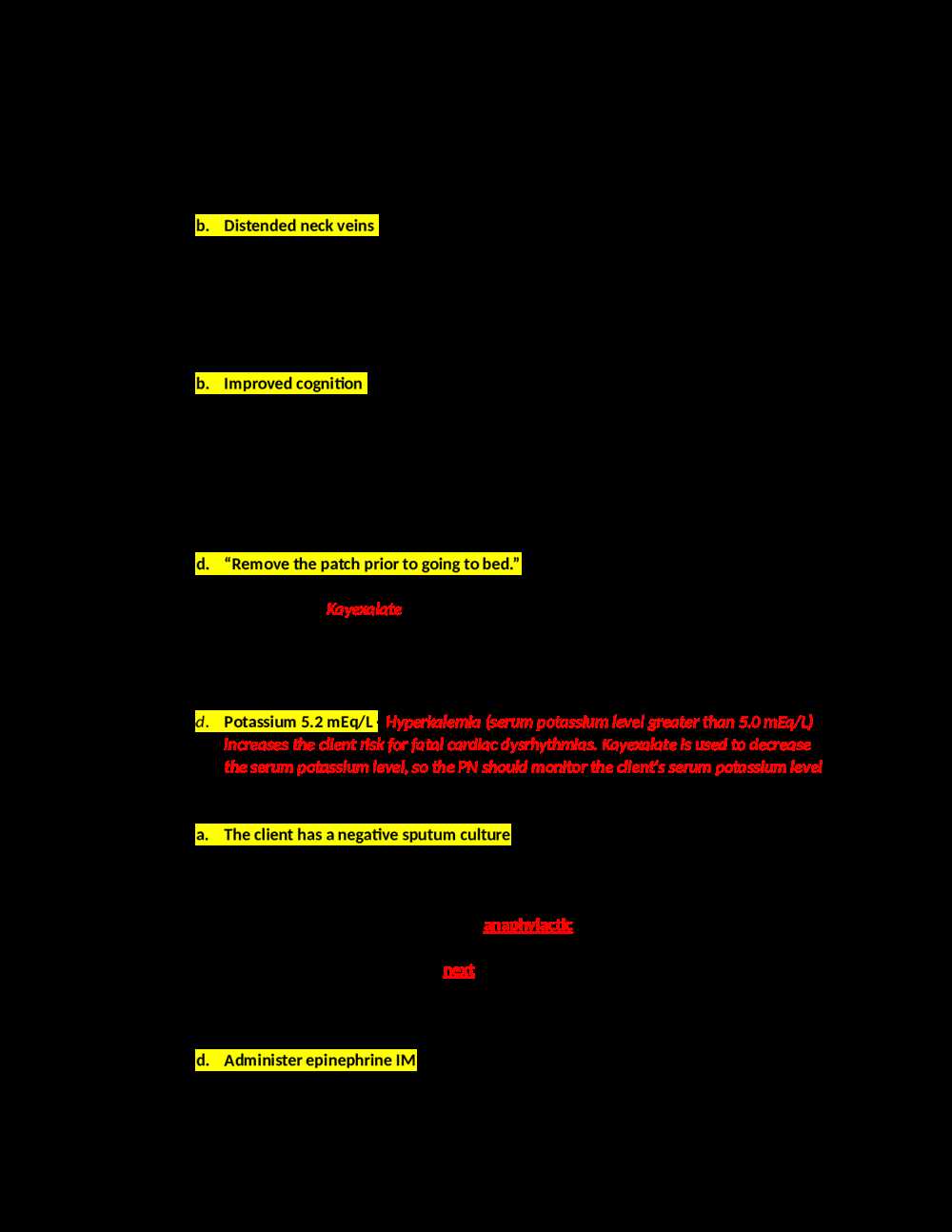
Another key area of focus for the ATI Pharmacology Exam 1 is understanding the nursing considerations for specific medications. These considerations include patient education, potential interactions with other drugs, and adverse effects to monitor for. By familiarizing yourself with these nursing considerations, you will be better equipped to answer questions related to patient care and medication management.
Overall, studying for an ATI Pharmacology Exam 1 requires a comprehensive understanding of drug classes, medication administration, and nursing considerations. By focusing on these key areas and developing a solid study plan, you can feel confident and well-prepared for the exam.
Overview of ATI Pharmacology Exam 1
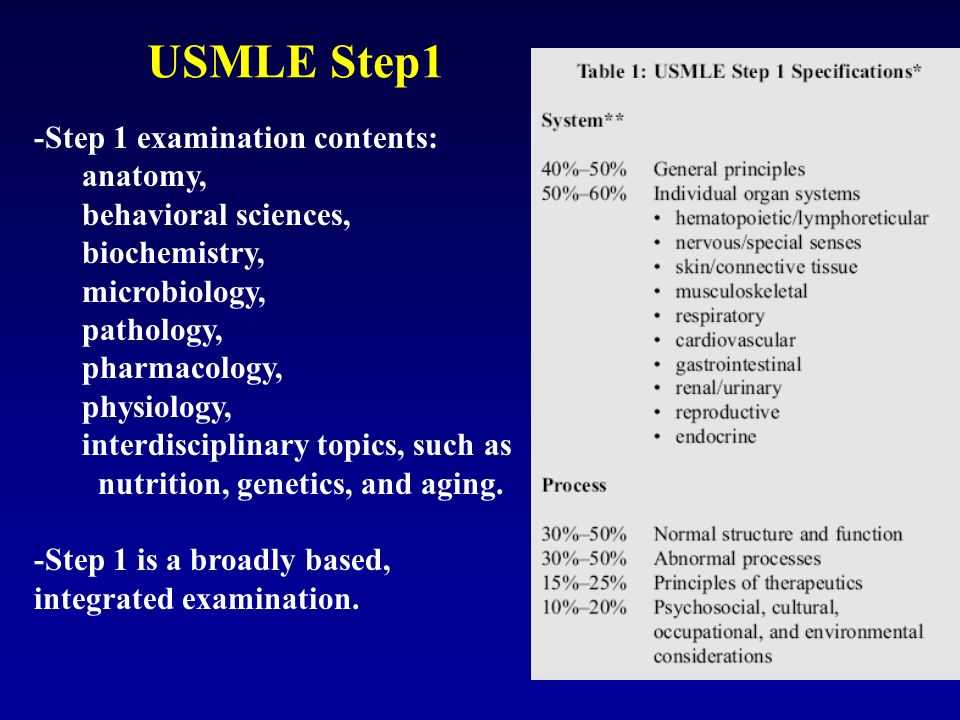
ATI Pharmacology Exam 1 is a comprehensive assessment that evaluates students’ knowledge and understanding of pharmacology principles and concepts. This exam covers a wide range of topics, including drug classes, medication administration, therapeutic effects, adverse effects, contraindications, and nursing implications.
The exam consists of multiple-choice questions that test students’ ability to apply pharmacological knowledge to real-life scenarios. The questions are designed to assess critical thinking skills, as well as the ability to prioritize nursing interventions and make clinical judgments.
Students preparing for the ATI Pharmacology Exam 1 should review key concepts and medication classes thoroughly. It is essential to understand the mechanism of action, indications, contraindications, and adverse effects of each drug class covered in the exam. Additionally, students should familiarize themselves with nursing interventions and considerations for each medication category.
- Key topics covered in ATI Pharmacology Exam 1 include:
- Pharmacokinetics and pharmacodynamics
- Medication administration and dosage calculations
- Adverse drug reactions and side effects
- Nursing implications and patient education
- Drug interactions and contraindications
- Medication safety and monitoring
Preparing for the exam requires a combination of studying and practice. It is recommended to utilize study guides, textbooks, and other resources to review the necessary content. Additionally, completing practice questions and simulations can help familiarize students with the types of scenarios they may encounter in the exam.
Overall, the ATI Pharmacology Exam 1 is a challenging assessment that requires a solid understanding of pharmacology principles and the ability to apply that knowledge to clinical situations. By thoroughly reviewing the key concepts and practicing with sample questions, students can enhance their chances of success on this exam.
Understanding the Basics of Pharmacology
Pharmacology is the study of drugs and their effects on the body. It is a branch of medicine that plays a crucial role in modern healthcare. To understand pharmacology, it is important to grasp the basics of the subject.
Drugs: Drugs are substances that alter the physiological processes in the body. They can be used for therapeutic purposes to treat diseases or relieve symptoms. Different drugs have different mechanisms of action and can target specific areas in the body.
Pharmacokinetics: Pharmacokinetics is the study of how drugs are absorbed, distributed, metabolized, and eliminated by the body. This includes understanding concepts such as bioavailability, half-life, and drug clearance. Pharmacokinetics helps determine the drug’s dosage and dosing intervals.
Pharmacodynamics: Pharmacodynamics is the study of how drugs exert their effects on the body and interact with specific receptors or target sites. It involves understanding concepts such as drug-receptor interactions, drug potency, and efficacy. Pharmacodynamics helps determine the optimal dose of a drug to achieve the desired therapeutic effect.
Adverse Drug Reactions: Adverse drug reactions are unwanted or harmful reactions that occur as a result of taking a medication. They can range from mild to severe and can occur due to various factors, including individual patient factors, drug-drug interactions, or drug allergies. Understanding adverse drug reactions is crucial for patient safety.
Drug Interactions: Drug interactions occur when two or more drugs interact with each other, altering their effects or causing unexpected side effects. It is important to understand potential drug interactions to avoid harm and ensure the effectiveness of medications. Some drug interactions can be managed by adjusting dosages or avoiding certain drug combinations.
Pharmacogenetics: Pharmacogenetics is the study of how an individual’s genetic makeup can influence their response to medications. Understanding pharmacogenetics can help personalize medicine by identifying individuals who may be at an increased risk of adverse drug reactions or those who may require dose adjustments for optimal therapeutic effects.
By gaining a solid understanding of the basics of pharmacology, healthcare professionals can make informed decisions about drug therapy, ensure patient safety, and optimize patient outcomes. Pharmacology forms the foundation of clinical practice and is essential in the field of medicine.
Pharmacokinetics and Pharmacodynamics
In the field of pharmacology, understanding pharmacokinetics and pharmacodynamics is crucial for the safe and effective use of medications. Pharmacokinetics refers to the study of how drugs are absorbed, distributed, metabolized, and eliminated by the body. This knowledge allows healthcare professionals to determine the appropriate dosage and frequency of drug administration.
Pharmacodynamics is concerned with how drugs interact with the body to produce their effects. This includes the mechanisms of action, receptor binding, and the relationship between drug concentration and response. Understanding pharmacodynamics helps clinicians predict the therapeutic and adverse effects of a drug, as well as identify potential drug interactions.
One important concept in pharmacokinetics is bioavailability, which refers to the fraction of an administered dose that reaches the systemic circulation. Factors such as drug formulation, route of administration, and first-pass metabolism can affect bioavailability. Monitoring blood levels of drugs can help assess their efficacy and guide dosage adjustments.
Pharmacodynamics can be explored through dose-response relationships, where the effect of a drug is plotted against its dosage. This allows for the determination of the minimum effective dose, maximum tolerated dose, and therapeutic index. Pharmacodynamics also considers the time course of drug effects, including onset, duration, and offset.
Overall, a thorough understanding of pharmacokinetics and pharmacodynamics is essential for healthcare professionals to optimize drug therapy and ensure patient safety. By considering how drugs are absorbed, distributed, metabolized, and eliminated, as well as how they interact with the body to produce their effects, clinicians can make informed decisions regarding drug selection, dosing, and monitoring.
Drug Categories and Classifications
Drug categories and classifications play a crucial role in the field of pharmacology. They help in organizing and categorizing medications based on their properties and therapeutic uses. Understanding drug categories and classifications is essential for healthcare professionals as it allows them to make informed decisions regarding the appropriate use of medications for their patients.
Drug Categories: Drugs are categorized into various groups based on their mechanism of action, therapeutic effect, chemical structure, and route of administration. Some common drug categories include analgesics, antibiotics, antineoplastics, cardiovascular drugs, central nervous system drugs, and immunosuppressants. Each drug category represents a specific class of medications with similar properties and therapeutic uses.
Drug Classifications: Within each drug category, medications are further classified based on their specific properties and characteristics. For example, within the analgesics category, drugs can be classified as non-opioid analgesics (such as acetaminophen and nonsteroidal anti-inflammatory drugs) or opioid analgesics (such as morphine and oxycodone). These classifications help healthcare professionals in selecting the most appropriate medication for a particular condition or symptom.
- Analgesics: Medications used to relieve pain. They can be classified as non-opioid or opioid analgesics.
- Antibiotics: Medications used to treat bacterial infections. They can be further classified based on their spectrum of activity and mechanism of action.
- Antineoplastics: Medications used in the treatment of cancer. They can be classified based on their mechanism of action and their specific targets in the cancer cells.
- Cardiovascular drugs: Medications used to treat cardiovascular conditions such as hypertension, heart failure, and arrhythmias. They can be classified based on their mechanism of action (e.g., beta blockers, calcium channel blockers) or their specific effects on the cardiovascular system.
- Central nervous system drugs: Medications used to treat conditions affecting the central nervous system, such as epilepsy, depression, and anxiety. They can be classified based on their mechanism of action (e.g., selective serotonin reuptake inhibitors, antiepileptic drugs) or their specific effects on the central nervous system.
- Immunosuppressants: Medications used to suppress the immune system. They are classified based on their mechanism of action and their specific targets in the immune system.
Overall, understanding drug categories and classifications is vital for healthcare professionals to ensure safe and effective medication management for their patients. It allows them to select the most appropriate medication based on the patient’s condition, consider potential drug interactions, and monitor for adverse effects. By having a comprehensive knowledge of drug categories and classifications, healthcare professionals can optimize patient outcomes and promote medication safety.
Understanding Drug Categories
For pharmacologists and healthcare professionals, understanding drug categories is an essential aspect of their practice. Drug categories refer to the classification of drugs based on their chemical structure, mode of action, therapeutic use, and potential adverse effects. This categorization helps in organizing drugs and simplifying their study and administration.
One of the commonly used drug classification systems is the Anatomical Therapeutic Chemical (ATC) classification system. It categorizes drugs into different levels based on their anatomical and therapeutic characteristics. The ATC system provides a hierarchical structure that starts with anatomical main groups (e.g., A for alimentary tract and metabolism) and further divides drugs into therapeutic subgroups and pharmacological subgroups.
Each drug category has its own set of characteristics and indications. For example, anticoagulants are drugs that inhibit blood clotting and are commonly used in the prevention and treatment of blood clots. Antiemetics, on the other hand, are drugs that help in relieving nausea and vomiting. Understanding these drug categories helps healthcare professionals tailor their treatment plans and select the appropriate medication for their patients.
Furthermore, knowing drug categories also helps in assessing potential drug interactions and adverse effects. For instance, drugs that belong to the same category may have similar mechanisms of action and thus increase the risk of drug interactions. Similarly, drugs within the same category may have similar adverse effects, allowing healthcare professionals to anticipate and manage potential side effects.
Summary:
- Understanding drug categories is important for pharmacologists and healthcare professionals.
- The Anatomical Therapeutic Chemical (ATC) classification system is commonly used to categorize drugs based on their anatomical and therapeutic characteristics.
- Each drug category has its own unique characteristics and indications.
- Knowing drug categories helps in tailoring treatment plans, selecting appropriate medications, and assessing potential drug interactions and adverse effects.
Common Drug Classifications
In the field of pharmacology, drugs are classified into different categories based on their mechanisms of action, therapeutic uses, and chemical structures. These drug classifications are essential for healthcare professionals, as they provide a framework for understanding and prescribing medications. Here are some common drug classifications:
- Antibiotics: Antibiotics are drugs that are used to treat bacterial infections. They work by inhibiting the growth or killing the bacteria. Common examples of antibiotics include penicillin, cephalosporins, and macrolides.
- Antidepressants: Antidepressants are medications used to treat depression and other mood disorders. They work by altering the balance of chemicals in the brain called neurotransmitters. Examples of antidepressants include selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs).
- Antihypertensives: Antihypertensives are drugs used to treat high blood pressure. They work by relaxing and widening the blood vessels, thus reducing the pressure within them. Examples of antihypertensives include angiotensin converting enzyme (ACE) inhibitors and calcium channel blockers.
- Anticoagulants: Anticoagulants, also known as blood thinners, are medications used to prevent the formation of blood clots. They work by interfering with the clotting process. Common examples of anticoagulants include warfarin and heparin.
Other common drug classifications include analgesics (pain relievers), antipsychotics, diuretics, and antidiabetic drugs. Each drug classification has its own specific properties and indications, and it is important for healthcare professionals to have a thorough understanding of these classifications to provide safe and effective patient care.