
In the field of biology and genetics, understanding the different types of human blood cells is crucial. Blood cell typing can be done to determine an individual’s blood type, which is important for various medical procedures including blood transfusions and organ transplants. POGIL, or Process Oriented Guided Inquiry Learning, is an educational method that promotes active learning through collaborative group work. In this article, we will explore the answers to commonly asked questions about human blood cell typing as part of a POGIL activity.
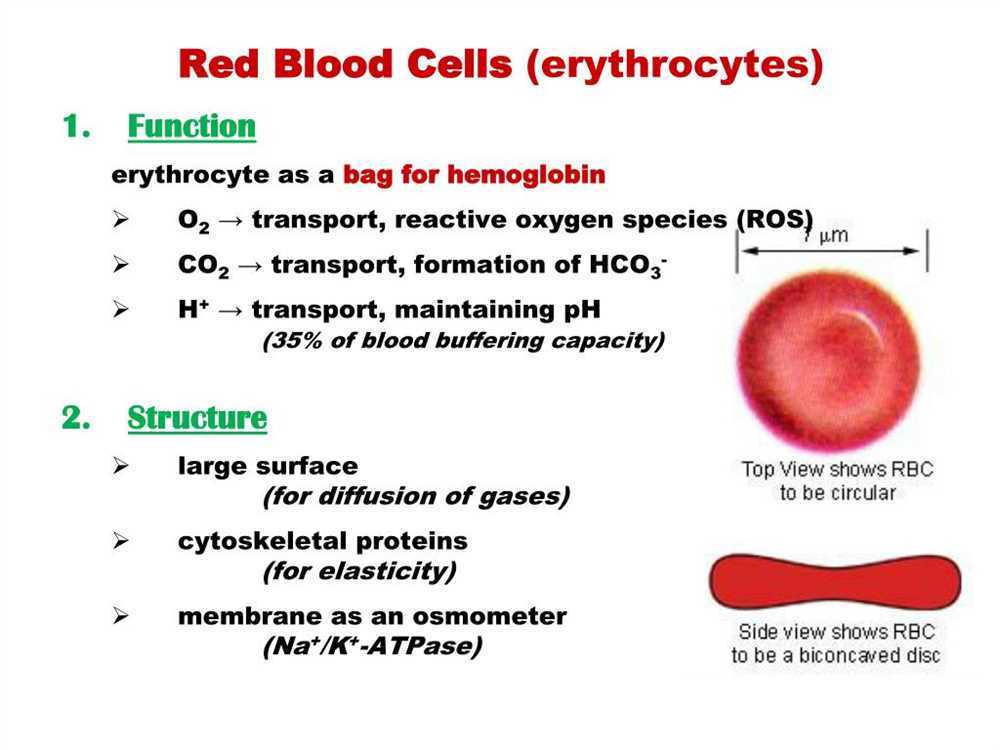
One of the first questions that may arise during a POGIL activity on blood cell typing is: what are the different types of human blood cells? It is important to note that blood is composed of several different types of cells, including red blood cells, white blood cells, and platelets. Red blood cells, also known as erythrocytes, are responsible for carrying oxygen throughout the body. White blood cells, or leukocytes, are involved in the immune response and help fight off infections. Platelets, on the other hand, play a role in blood clotting to prevent excessive bleeding.
Another question that may be asked is: what are the different blood types in humans? Human blood can be categorized into different blood types, including A, B, AB, and O. These blood types are determined by the presence or absence of certain antigens on the surface of red blood cells. For example, individuals with blood type A have the A antigen, those with blood type B have the B antigen, individuals with blood type AB have both A and B antigens, and individuals with blood type O have neither A nor B antigens.
Furthermore, a common question during a POGIL activity on blood cell typing may be: how is blood typing performed in a laboratory setting? Blood typing is typically done using a technique called serological typing. This involves mixing the individual’s blood sample with known antibodies that will react specifically with certain antigens. By observing whether or not the blood sample clumps or agglutinates, the technician can determine the individual’s blood type. For example, if a blood sample agglutinates when mixed with anti-A antibodies but does not agglutinate with anti-B antibodies, the individual is blood type A.
In conclusion, blood cell typing is an essential part of understanding human blood and its different types. Through POGIL activities, students can actively engage in the learning process and gain a deeper understanding of the topic. By exploring questions such as the different types of blood cells, the different blood types in humans, and the laboratory techniques used for blood typing, students can develop a comprehensive understanding of human blood cell typing.
Understanding the Basics of Human Blood Cell Typing
Human blood cell typing is the process of determining the specific characteristics of an individual’s blood cells. This information is important in various medical procedures, including blood transfusions, organ transplants, and genetic testing. The typing process involves identifying various cell surface markers or antigens on red blood cells, white blood cells, and platelets, which are used to classify blood into different types.
Red blood cell typing:
The most well-known system for classifying red blood cells is the ABO blood group system. This system categorizes blood into four main types: A, B, AB, and O. The classification is based on the presence or absence of certain antigens on the surface of red blood cells. For example, individuals with blood type A have the A antigen, while those with blood type B have the B antigen. Those with type AB have both antigens, and those with type O have neither.
In addition to the ABO system, there is another important antigen called the Rh factor. This antigen determines whether an individual’s blood is classified as Rh positive or Rh negative. Rh positive individuals have the Rh antigen on their red blood cells, while Rh negative individuals do not. Combining the ABO and Rh factors results in the eight main blood types: A+, A-, B+, B-, AB+, AB-, O+, and O-.
White blood cell typing:
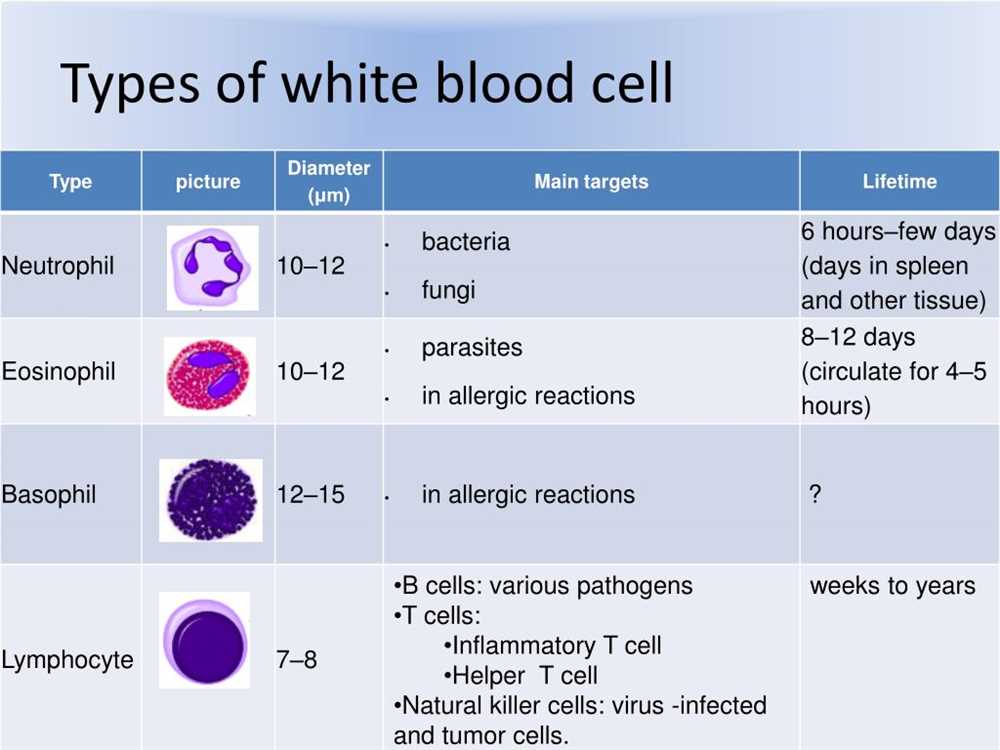
Unlike red blood cells, white blood cells do not have a specific blood typing system like the ABO system. However, there are various subtypes of white blood cells that can be identified and classified based on specific antigens. White blood cell typing is often used in the diagnosis and monitoring of various diseases, including leukemia and autoimmune disorders.
Platelet typing:
Platelets, which are involved in blood clotting, can also be typed based on specific antigens. This information is important in determining the compatibility of platelets for transfusions. Platelet typing involves identifying antigens such as HPA (human platelet antigens), which are associated with various platelet disorders and immune responses.
In conclusion, human blood cell typing plays a crucial role in various medical procedures and treatments. Understanding the basics of blood cell typing, including the ABO system, Rh factor, and the typing of white blood cells and platelets, is essential for ensuring the safety and compatibility of blood transfusions, organ transplants, and other medical interventions.
The ABO Blood Group System: Key Concepts and Significance
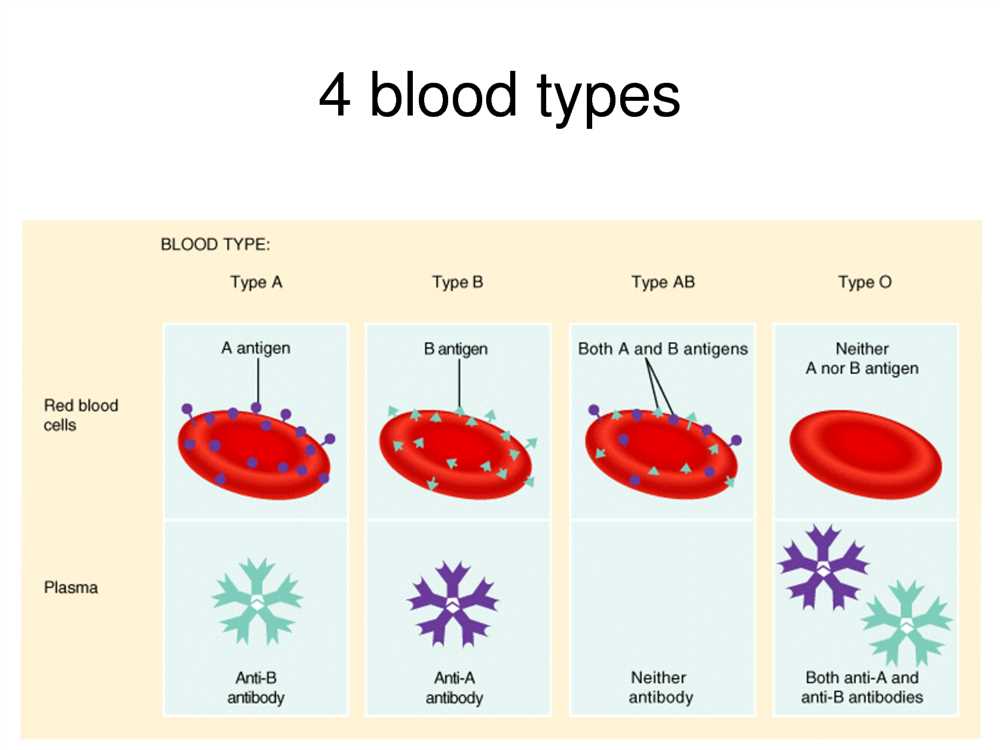
The ABO blood group system is the most well-known and important blood typing system used in humans. It classifies blood into four main groups: A, B, AB, and O. These groups are determined by the presence or absence of A and B antigens on the surface of red blood cells. The presence of both A and B antigens results in blood type AB, the absence of both antigens leads to blood type O, and the presence of either A or B antigen results in blood types A or B, respectively.
The ABO blood groups are of crucial significance in blood transfusion and organ transplantation. It is essential to match the blood types of the donor and recipient to prevent adverse reactions. For example, individuals with blood type A can only receive blood from donors with type A or O, whereas individuals with blood type B can receive blood from donors with type B or O. Blood type AB individuals, being universal recipients, can receive blood from any blood type, while those with blood type O are universal donors and can donate blood to individuals with any blood type.
Moreover, the ABO blood group system has implications beyond blood transfusion. It plays a role in paternity testing, as it can determine the biological relationship between a child and potential father. Additionally, the ABO blood groups are associated with certain health conditions and diseases, such as increased susceptibility to certain infections or an increased risk of heart disease. Therefore, understanding and considering the ABO blood group system is crucial in various medical and forensic contexts.
Overview of the ABO Blood Group System
The ABO blood group system is one of the most well-known and widely studied blood group systems in human biology. It is based on the presence or absence of specific antigens on the surface of red blood cells, which are determined by the ABO gene. The system classifies blood into four major types: A, B, AB, and O.
The A and B antigens are glycoproteins that are encoded by the ABO gene. If an individual has the A antigen on their red blood cells, they are assigned blood type A. If they have the B antigen, they are assigned blood type B. If they have both A and B antigens, they are assigned blood type AB. If they have neither A nor B antigens, they are assigned blood type O.
The ABO blood group system also involves the presence of antibodies in plasma, which are proteins that recognize and bind to specific antigens. Individuals with blood type A have anti-B antibodies in their plasma; those with blood type B have anti-A antibodies; those with blood type AB have neither antibody; and those with blood type O have both anti-A and anti-B antibodies.
The ABO blood group system is important in determining blood compatibility for transfusions and organ transplantation. Blood type A can safely receive blood from type A or type O donors, while blood type B can safely receive blood from type B or type O donors. Blood type AB is considered the universal recipient and can receive blood from any blood type, while blood type O is considered the universal donor and can donate blood to any blood type.
Role of ABO Blood Group Typing in Transfusions and Organ Transplants
ABO blood group typing is a crucial step in ensuring successful transfusions and organ transplants. The ABO blood group system is based on the presence or absence of certain antigens on the surface of red blood cells. These antigens are designated as A, B, or AB, and individuals with no antigens are classified as type O. The presence or absence of these antigens determines compatibility for transfusion or transplantation.
During a transfusion, matching the ABO blood type of the donor and recipient is essential to prevent adverse reactions. If a patient receives blood with a different ABO blood type, the recipient’s immune system will recognize the foreign antigens as invaders and mount an immune response. This can lead to severe complications, such as hemolysis (destruction of red blood cells) and kidney failure. Therefore, blood banks carefully screen donors and recipients to ensure compatibility.
Similarly, ABO blood group typing plays a critical role in organ transplantation. The ABO blood type of the donor and recipient must match for a successful transplant. If a patient receives an organ from a donor with a different blood type, the recipient’s immune system will recognize the foreign antigens on the transplanted organ and reject it. This can result in organ failure and the need for re-transplantation. Therefore, organ transplant centers prioritize ABO blood typing to increase the likelihood of a successful outcome.
In summary, ABO blood group typing is essential in transfusions and organ transplants to ensure compatibility and prevent adverse reactions. By accurately matching the blood type of donors and recipients, healthcare professionals can minimize the risk of complications and improve patient outcomes. ABO blood group typing is a simple yet vital step in the process of delivering safe and effective transfusions and organ transplants.
The Rh Blood Group System: Understanding Rh Factor and Typing
The Rh blood group system is an important aspect of human blood typing that involves the presence or absence of specific antigens on the surface of red blood cells. Rh factor, also known as Rhesus factor, is named after the Rhesus monkey in which it was first discovered. Understanding the Rh blood group system and typing is crucial in blood transfusions and pregnancy management.
The Rh factor is determined by the presence or absence of the Rh antigens on the surface of red blood cells. Individuals who have these antigens are Rh positive, while those who lack them are Rh negative. The most common Rh antigen is called D antigen. Therefore, individuals who are Rh positive have the D antigen on their red blood cells.
There are several methods for typing Rh blood groups, including the direct agglutination test, the indirect antiglobulin test, and molecular methods. The direct agglutination test involves mixing the patient’s blood with anti-Rh antibodies to see if agglutination or clumping occurs. If agglutination occurs, it means the person is Rh positive. The indirect antiglobulin test is used to detect the presence of Rh antibodies in a person’s blood. This test is often used to determine blood compatibility for transfusions or to determine if an Rh negative woman is at risk of Rh incompatibility during pregnancy. Molecular methods involve analyzing the individual’s DNA to determine their Rh factor.
Knowing a person’s Rh blood type is essential in medical procedures. For example, in blood transfusions, it is crucial to match the Rh type of the donor and recipient to prevent adverse reactions. In pregnancy, an Rh negative woman carrying an Rh positive fetus may develop Rh sensitization, where her immune system produces antibodies against the Rh antigens. These antibodies can cross the placenta and attack the red blood cells of future Rh positive pregnancies, potentially causing severe complications.
In conclusion, understanding the Rh blood group system and typing is vital in various medical situations. It allows for safe and compatible blood transfusions and enables healthcare professionals to manage pregnancies effectively. By determining an individual’s Rh factor, healthcare providers can take appropriate precautions and provide the necessary interventions to ensure the best possible outcomes for patients.
Significance of Rh Typing in Pregnancy and Blood Transfusions
Rh typing is a vital component in prenatal care and blood transfusions to prevent potential complications and ensure the safety of the patient. The Rh antigen, also known as the Rh factor, is a protein found on the surface of red blood cells. It plays a crucial role in determining blood compatibility between individuals, especially during pregnancy and transfusion procedures.
In pregnancy, Rh typing is particularly important to assess the Rh compatibility between the mother and fetus. If the mother is Rh negative and the fetus is Rh positive, there is a risk of Rh incompatibility occurring. This can lead to the production of antibodies by the mother’s immune system against the Rh factor, potentially causing complications in subsequent pregnancies. Rh negative mothers who are found to have Rh-positive fetuses may require specific interventions, such as Rh immunoglobulin administration, to prevent the development of these antibodies and protect future pregnancies.
In the context of blood transfusions, Rh typing is critical to avoid adverse reactions in recipients. If an Rh-negative individual receives Rh-positive blood, their immune system may produce antibodies against the Rh factor, leading to hemolytic reactions. These reactions can range from mild to severe, even life-threatening in some cases. Therefore, it is essential to match the Rh type of the donor and recipient to prevent such reactions and ensure the overall safety and effectiveness of the transfusion.
Overall, Rh typing is of utmost importance in both pregnancy and blood transfusion settings. It allows healthcare professionals to identify potential risks, take appropriate preventive measures, and ensure the well-being of patients. By accurately determining the Rh type and considering compatibility, healthcare providers can minimize complications and enhance the success of both prenatal care and blood transfusion procedures.