Pathophysiology Exam 1 is a crucial assessment in the field of healthcare and medical sciences. This exam focuses on understanding the underlying mechanisms of diseases, their progression, and the effects they have on the human body. Students undertaking this exam at Rasmussen College are required to demonstrate their knowledge and understanding of various concepts related to pathophysiology in order to excel in their academic pursuits.
The exam covers a wide range of topics, including cellular adaptations, inflammation, immunity, and alterations in tissue integrity. Students are expected to demonstrate their understanding of the pathophysiological processes that occur in different disease states and their impact on the body’s homeostasis. They are also required to analyze and interpret clinical data, as well as apply critical thinking skills to make effective clinical judgments.
Preparing for Pathophysiology Exam 1 requires dedicated study and review of the course material. Students are encouraged to develop a comprehensive understanding of the underlying principles of pathophysiology, as well as the application of this knowledge in clinical settings. This includes understanding the signs and symptoms of various diseases, their etiology, and the diagnostic and treatment modalities used to manage them.
Successfully passing Pathophysiology Exam 1 at Rasmussen College is an important milestone for students pursuing careers in the healthcare field. It demonstrates their ability to apply their theoretical knowledge in a practical setting and their competence in understanding the complex mechanisms of diseases. This exam serves as a foundation for further studies in pathophysiology and prepares students for their future professional endeavors in healthcare.
Overview of Pathophysiology
Pathophysiology is the study of the functional changes that occur in the body as a result of disease or injury. It examines how these changes disrupt the normal functioning of organs and systems, leading to the development of specific signs and symptoms. By understanding the underlying mechanisms of disease, healthcare professionals can better diagnose and treat patients.
Causes of Pathophysiology: Pathophysiology can be caused by a variety of factors, including genetic mutations, infections, toxins, and trauma. These factors can disrupt cellular processes, alter enzyme function, and interfere with the body’s ability to maintain homeostasis.
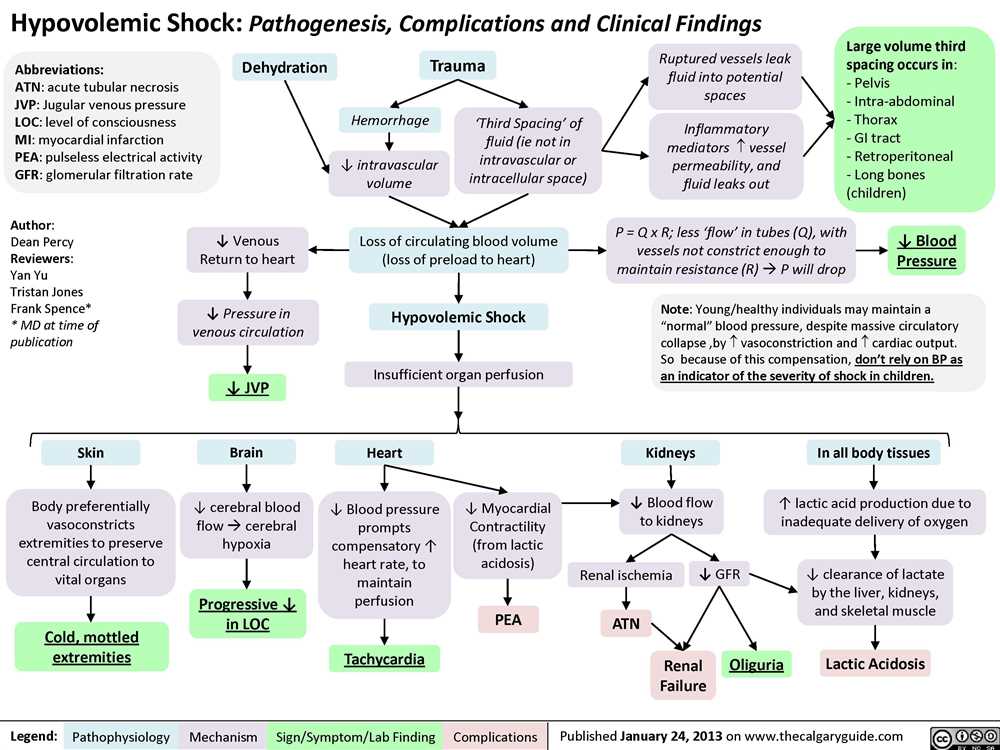
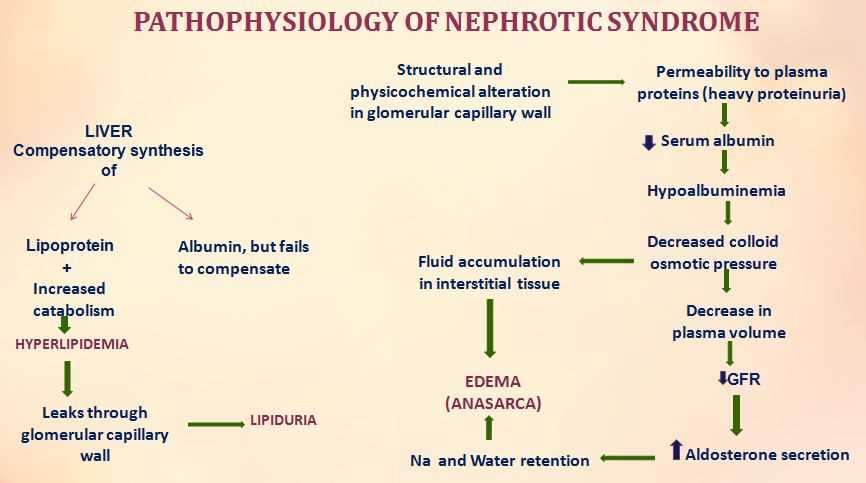
Effects on Organ Systems: The effects of pathophysiology can vary depending on the organ system involved. For example, in cardiovascular pathophysiology, disruptions in blood flow can lead to conditions such as hypertension, congestive heart failure, or myocardial infarction. Similarly, respiratory pathophysiology can result in conditions like asthma or chronic obstructive pulmonary disease.
Common Pathophysiological Conditions: There are numerous pathophysiological conditions that healthcare professionals encounter on a regular basis. These include diabetes mellitus, cancer, autoimmune disorders, infectious diseases, and neurological disorders such as Alzheimer’s and Parkinson’s disease.
Diagnosis and Treatment: Diagnosis of pathophysiological conditions often involves a combination of patient history, physical examination, laboratory tests, and imaging studies. Treatment options vary depending on the specific condition but may include medication, surgery, lifestyle changes, and supportive care.
Importance of Pathophysiology: Pathophysiology is an essential component of healthcare education and practice. It provides a foundation for understanding disease processes, allows for early detection and intervention, and guides evidence-based treatment decisions. By studying pathophysiology, healthcare professionals can improve patient outcomes and contribute to the advancement of medical knowledge.
References:
- McCance, K. L., & Huether, S. E. (2018). Pathophysiology: The biologic basis for disease in adults and children. Elsevier Health Sciences.
- Huether, S. E., & McCance, K. L. (2014). Understanding pathophysiology. Elsevier Health Sciences.
Importance of Exam 1 in Pathophysiology
The first exam in Pathophysiology is of utmost importance for several reasons. Firstly, it serves as a benchmark for evaluating students’ understanding and grasp of the fundamental concepts and mechanisms underlying disease processes. The exam tests the students’ ability to apply the knowledge they have acquired during the course lectures, readings, and discussions to analyze and interpret clinical scenarios.
Secondly, the exam assesses the students’ ability to critically think and reason through complex pathophysiological problems and develop appropriate strategies for diagnosis, management, and treatment. It challenges students to think beyond rote memorization and encourages them to develop problem-solving skills that are essential in the clinical setting.
Furthermore, the exam helps identify areas of strengths and weaknesses in students’ knowledge and understanding of pathophysiology. This feedback is crucial for both students and instructors, as it allows them to focus on areas that require further study and improvement. It also provides an opportunity for students to reflect on their study strategies and make necessary adjustments to enhance their learning and performance.
Additionally, the first exam sets the tone for the rest of the course and establishes a solid foundation for subsequent topics. By successfully passing the exam, students demonstrate their readiness to delve deeper into advanced concepts and build upon the knowledge gained in the previous modules. It gives them the confidence and motivation to continue their learning journey in Pathophysiology.
In conclusion, the first exam in Pathophysiology holds significant importance in assessing students’ understanding, critical thinking skills, and ability to apply knowledge to real-life scenarios. It serves as a crucial tool for self-evaluation, identifying areas of improvement, and establishing a strong foundation for further learning. Success in the exam sets the stage for future success in the course and prepares students for the challenges they will encounter in their healthcare careers.
Key Topics Covered in Pathophysiology Exam 1
Pathophysiology Exam 1 covers several important topics related to the study of disease processes in the body. These topics include:
- The general principles of pathophysiology
- Cellular adaptations and cell injury
- Inflammation and tissue repair
- Genetic disorders and inherited diseases
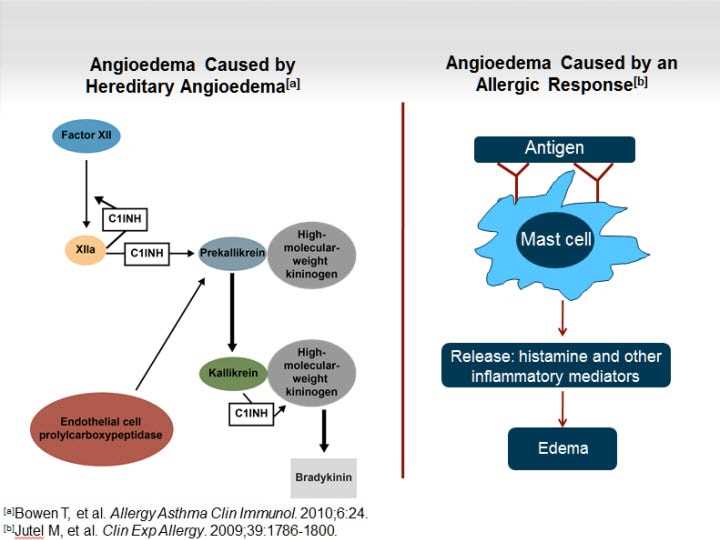
- Immunological disorders and hypersensitivity reactions
- Cancer and oncogenesis
During the exam, students will be tested on their understanding of these key topics and their ability to apply the knowledge to clinical scenarios. They will be expected to demonstrate a thorough understanding of the underlying mechanisms of disease and how they manifest in the body.
Additionally, the exam may also include questions on the diagnostic methods and treatment options associated with various diseases. Students are encouraged to review their course materials, including lecture notes, textbooks, and any additional resources provided by the instructor, to thoroughly prepare for the exam.
Cellular Adaptation
Cellular adaptation refers to the ability of cells to modify their structure or function in response to changes in their environment. It is a fundamental process that allows cells to maintain homeostasis and to respond to stressors or injuries. There are several types of cellular adaptations, including hypertrophy, hyperplasia, atrophy, metaplasia, and dysplasia. These adaptations can occur in various tissues and organs throughout the body.
Hypertrophy is an increase in the size of cells, leading to an increase in the size of the affected organ or tissue. This can occur in response to increased workload or hormonal stimulation. For example, skeletal muscle hypertrophy can occur as a result of exercise or weightlifting.
Hyperplasia refers to an increase in the number of cells in an organ or tissue. This can occur in response to hormonal stimulation or tissue damage. For example, the uterus undergoes hyperplasia during pregnancy.
Atrophy is a decrease in the size and function of cells, leading to a decrease in the size of the affected organ or tissue. This can occur due to disuse, decreased blood supply, or hormonal or nutritional deficiencies. For example, skeletal muscle atrophy can occur in individuals who are bedridden.
Metaplasia is a reversible change in which one adult cell type is replaced by another cell type. This can occur in response to chronic irritation or inflammation. For example, the epithelial cells in the respiratory tract of smokers can undergo metaplasia and change from ciliated columnar cells to squamous cells.
Dysplasia is an abnormal growth or development of cells, leading to changes in cell size, shape, and organization. It is often considered a pre-cancerous condition. Dysplasia can occur in response to chronic irritation or inflammation. For example, cervical dysplasia can occur as a result of human papillomavirus (HPV) infection.
In conclusion, cellular adaptation is a crucial process that allows cells to respond and adapt to changes in their environment. These adaptations can be beneficial, such as in the case of hypertrophy or hyperplasia, or they can be detrimental, such as in the case of atrophy, metaplasia, or dysplasia. Understanding the mechanisms of cellular adaptation is essential for understanding the pathophysiology of various diseases and for developing effective treatment strategies.
Inflammation and Immunity
Inflammation is a complex biological response to tissue damage or infection and is an integral part of the body’s defense mechanism. It involves various cells, mediators, and cytokines that work together to eliminate the harmful stimulus and initiate the process of healing. The immune system plays a crucial role in inflammation by recognizing foreign substances and mounting an immune response to eliminate them.
When tissue damage occurs, the immune system recognizes it and initiates an inflammatory response. This response involves the release of inflammatory mediators, such as histamine, prostaglandins, and cytokines, which cause vasodilation, increased blood flow, and increased vascular permeability. These changes result in the redness, heat, swelling, and pain that are characteristic of inflammation.
The immune system is also responsible for recognizing and eliminating foreign substances, such as pathogens or toxins, through the process of immunity. It does this through the activation of various components, including phagocytes, lymphocytes, and antibodies. Phagocytes, such as neutrophils and macrophages, engulf and destroy pathogens, while lymphocytes, such as T cells and B cells, target specific antigens and initiate an immune response. Antibodies, produced by B cells, bind to antigens and mark them for destruction by phagocytes or complement proteins.
Inflammation and immunity are closely interconnected processes. Inflammation provides the initial response to tissue damage or infection, while immunity ensures long-term protection against pathogens. By understanding the mechanisms underlying inflammation and immunity, healthcare professionals can better identify and treat various diseases and conditions that involve these processes.
Tissue Repair and Wound Healing
When tissues in the body are injured or damaged, the body initiates a complex process called tissue repair and wound healing. This process involves various cell types, molecules, and signaling pathways to restore the structure and function of the damaged tissue.
One of the key players in tissue repair is the inflammatory response. After injury, damaged cells release chemical signals that attract immune cells to the site of injury. These immune cells, such as neutrophils and macrophages, help remove debris and pathogens, and produce cytokines that initiate the healing process. In addition, platelets are activated and release growth factors that stimulate the proliferation of new cells.
During the healing process, different cell types are involved, including fibroblasts, which produce collagen to create a temporary scaffold for new tissue formation. As the wound heals, new blood vessels are formed through angiogenesis, supplying oxygen and nutrients to the healing tissue. Epithelial cells migrate and undergo proliferation to cover the wound and restore the barrier function of the skin or mucous membranes.
There are two types of wound healing: primary intention and secondary intention. Primary intention healing occurs when the wound edges are brought together, such as in a surgical incision. Secondary intention healing occurs when the wound edges cannot be directly approximated, such as in a pressure ulcer or a large laceration. In secondary intention healing, the wound fills with granulation tissue, which eventually contracts to reduce the size of the wound.
In summary, tissue repair and wound healing are complex processes involving inflammation, cell proliferation, and tissue remodeling. The coordinated actions of various cell types and molecules are necessary for optimal healing. Understanding the underlying mechanisms of tissue repair is crucial for developing effective treatments for wounds and promoting optimal healing outcomes.
Genetic and Developmental Disorders
Genetic and developmental disorders are conditions that are caused by abnormalities in genes or disruptions in the normal process of development. These disorders can have a wide range of effects on an individual’s health and development, and may manifest in various ways depending on the specific genetic or developmental defect.
One example of a genetic disorder is Down syndrome, which is caused by the presence of an extra copy of chromosome 21. This extra genetic material leads to developmental delays, intellectual disability, and characteristic physical features. Another genetic disorder is cystic fibrosis, which is caused by mutations in the CFTR gene. This disorder affects the production of mucus and leads to problems in the respiratory and digestive systems.
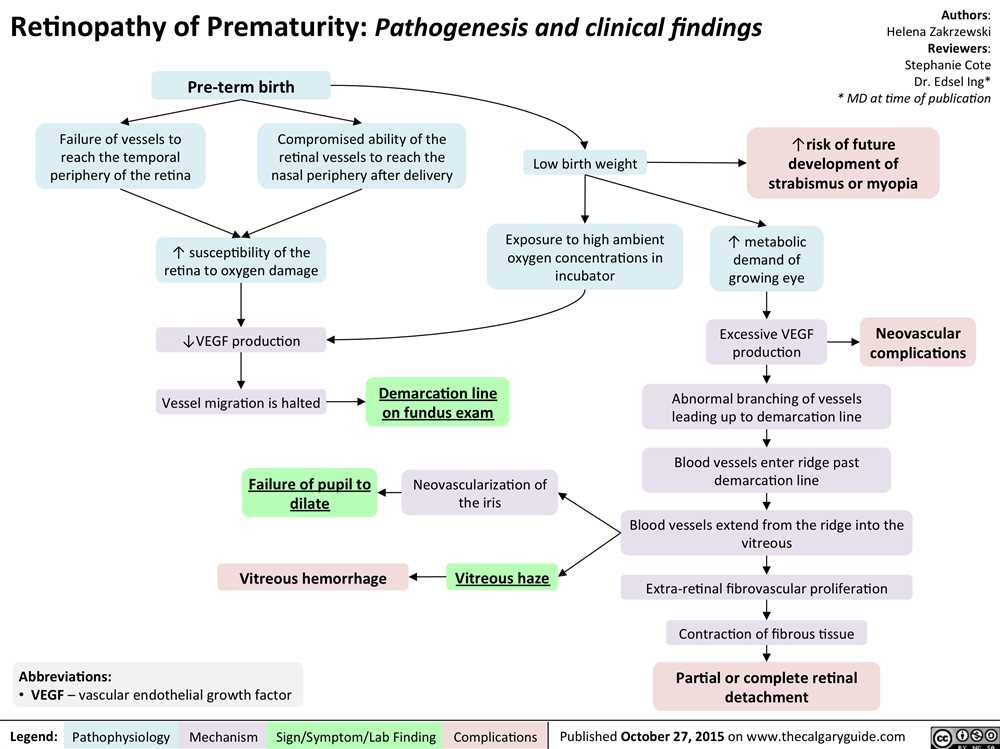
Developmental disorders can also be caused by factors such as exposure to toxins or infections during pregnancy, or by problems with the development of the brain or other organs. For example, fetal alcohol syndrome is a developmental disorder that is caused by maternal alcohol consumption during pregnancy. This condition can result in growth delays, facial abnormalities, and cognitive and behavioral issues.
Diagnosing and managing genetic and developmental disorders often involves a combination of physical examinations, genetic testing, and medical interventions. Treatment options may include medications, therapies, and surgeries, depending on the specific disorder and its effects on the individual’s health and development. Early intervention and ongoing support are key in managing these disorders and optimizing the affected individual’s quality of life.