Pathophysiology Exam 2 is a comprehensive assessment that evaluates students’ understanding of the underlying mechanisms of disease. This exam delves into the intricate details of how normal physiological processes become disrupted and lead to the development of various diseases.
During Exam 2, students are tested on their knowledge of cellular malfunction, altered tissue integrity, and the pathogenesis of specific diseases. This exam provides a deeper understanding of the pathophysiological processes behind conditions such as cancer, cardiovascular diseases, respiratory disorders, and autoimmune disorders.
By examining the mechanisms of disease at a cellular and molecular level, this exam allows students to connect the dots between normal physiology and abnormal pathology. It challenges students to apply their knowledge of various regulatory mechanisms, such as inflammation, immune response, and genetic factors, to the development and progression of diseases.
Understanding Pathophysiology Exam 2: A Comprehensive Guide
Preparing for a pathophysiology exam can be daunting, especially when it comes to exam 2, which covers a wide range of topics. However, with a comprehensive guide and understanding of key concepts, you can approach the exam with confidence. In this guide, we will delve into the important points that you need to know for exam 2 of pathophysiology.
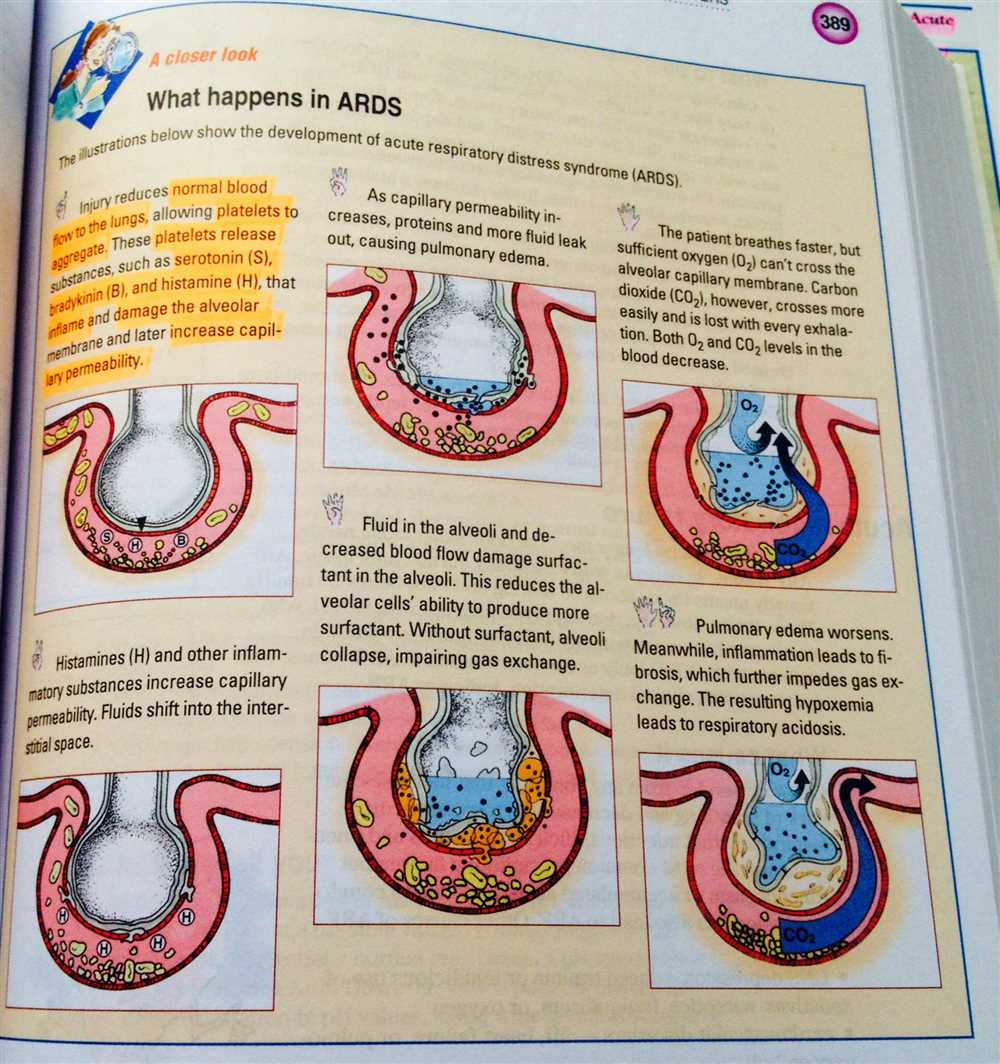
1. Respiratory System Disorders: One of the key areas covered in exam 2 is respiratory system disorders. This includes understanding the pathophysiology of conditions such as asthma, chronic obstructive pulmonary disease (COPD), pneumonia, and acute respiratory distress syndrome (ARDS). Familiarize yourself with the underlying mechanisms of these disorders, including airway inflammation, bronchoconstriction, and impaired gas exchange. Also, study the clinical manifestations, diagnostic tests, and treatment options for each condition.
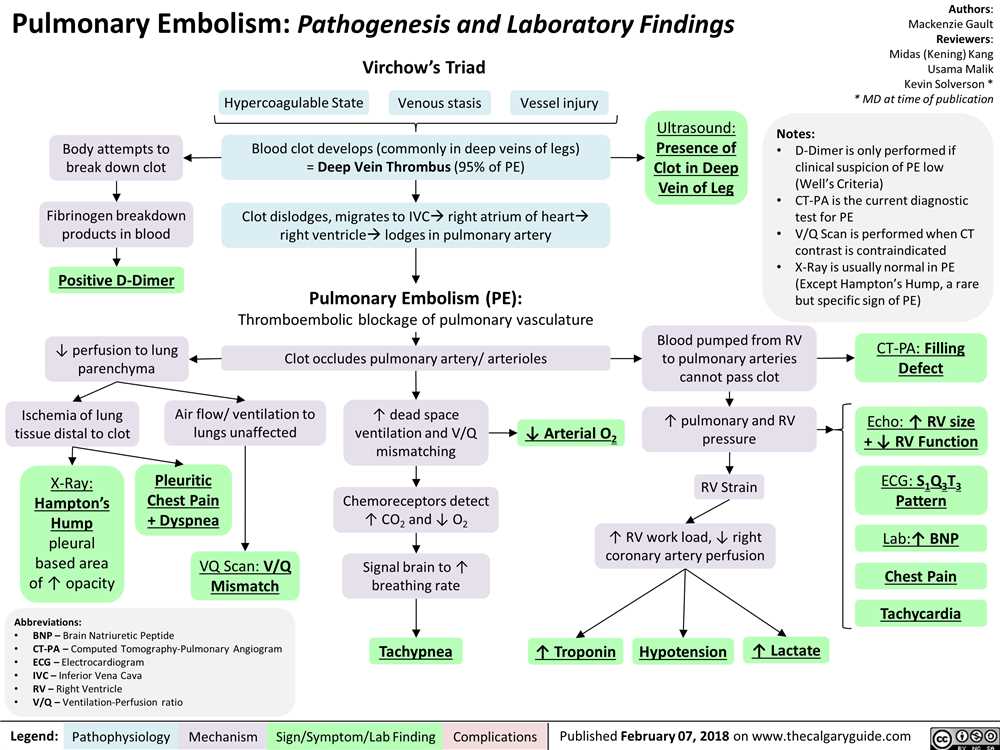
2. Cardiovascular System Disorders: Another important topic in exam 2 is cardiovascular system disorders. This includes understanding the pathophysiology of conditions such as hypertension, coronary artery disease (CAD), heart failure, and arrhythmias. Focus on the underlying mechanisms of these disorders, such as endothelial dysfunction, atherosclerosis, and myocardial remodeling. Also, study the clinical manifestations, diagnostic tests, and treatment approaches for each condition.
3. Renal System Disorders: Exam 2 may also cover renal system disorders. This includes understanding the pathophysiology of conditions such as acute kidney injury (AKI), chronic kidney disease (CKD), nephrotic syndrome, and urinary tract infections (UTIs). Pay attention to the underlying mechanisms of these disorders, including renal ischemia, glomerular damage, and urinary stasis. Also, study the clinical manifestations, diagnostic tests, and management strategies for each condition.
4. Endocrine System Disorders: Lastly, exam 2 may test your knowledge on endocrine system disorders. This includes understanding the pathophysiology of conditions such as diabetes mellitus, thyroid disorders, adrenal gland disorders, and pituitary gland disorders. Focus on the underlying mechanisms of these disorders, such as insulin resistance, hormone imbalances, and glandular dysfunction. Also, study the clinical manifestations, diagnostic tests, and treatment options for each condition.
By thoroughly studying and understanding these key topics, you can confidently tackle exam 2 of pathophysiology. Remember to review the fundamental concepts, delve into the underlying mechanisms, and familiarize yourself with the clinical manifestations and management strategies for each disorder. Good luck!
Overview of Pathophysiology Exam 2
Throughout the exam, you can expect to encounter questions that require a comprehensive understanding of the underlying causes, progression, and complications of different diseases. You will need to apply your knowledge of cellular and molecular processes, as well as systemic responses, to analyze and interpret various clinical scenarios.
- Disease Processes: One of the key areas covered in this exam is the detailed study of specific diseases and disorders. You will explore the etiology, pathogenesis, and clinical manifestations of conditions such as cardiovascular diseases, respiratory disorders, immune system abnormalities, and neurological disorders.
- Pathophysiological Mechanisms: Another important aspect of the exam is understanding the mechanisms that drive disease progression. This includes a deep dive into cellular and molecular processes, such as inflammation, immune responses, genetic mutations, and dysregulation of homeostasis.
- Clinical Application: A crucial skill that you will develop during this exam is the ability to apply your knowledge of pathophysiology to real-life clinical scenarios. You will be presented with case studies and asked to analyze symptoms, interpret diagnostic tests, and propose appropriate treatment strategies based on your understanding of disease processes.
To excel in Pathophysiology Exam 2, it is important to study and review a wide range of topics, including cellular biology, genetics, immunology, and the physiological systems of the body. Pay close attention to the interconnectedness of different body systems and how disturbances in one system can impact the overall health of an individual. Good luck with your preparation for the exam!
Respiratory System Disorders
The respiratory system is responsible for the exchange of oxygen and carbon dioxide in the body. When this system is disrupted, it can lead to various disorders and diseases. One common disorder is asthma, which is characterized by inflammation and narrowing of the airways. It is often triggered by allergens, such as dust or pollen, and can result in wheezing, coughing, and shortness of breath.
Another respiratory disorder is chronic obstructive pulmonary disease (COPD), which includes conditions such as chronic bronchitis and emphysema. COPD is often caused by long-term exposure to irritants, such as smoking or air pollution. It leads to the progressive deterioration of lung function, making it difficult for individuals to breathe properly.
In addition to asthma and COPD, respiratory infections are also common. These infections can affect the upper respiratory tract, such as the common cold or sinusitis, or the lower respiratory tract, such as pneumonia or bronchitis. They are often caused by viral or bacterial pathogens and can result in symptoms such as cough, congestion, and fever.
Lung cancer is another serious respiratory disorder that can develop due to factors such as smoking, exposure to environmental toxins, or genetic predisposition. It is characterized by the uncontrolled growth of abnormal cells in the lungs and can lead to symptoms such as chest pain, coughing up blood, and weight loss.
Overall, respiratory system disorders can significantly impact an individual’s quality of life and require appropriate diagnosis and treatment. It is important to protect the respiratory system by avoiding exposure to irritants and maintaining a healthy lifestyle.
Cardiovascular System Disorders
The cardiovascular system is responsible for circulating blood throughout the body, delivering oxygen and nutrients to the cells and removing waste products. However, there are several disorders that can affect the normal function of the cardiovascular system. These disorders can range from minor inconveniences to life-threatening conditions.
One of the most common disorders of the cardiovascular system is hypertension, or high blood pressure. Hypertension occurs when the force of blood against the artery walls is consistently too high, leading to increased stress on the heart and blood vessels. This can eventually lead to serious complications such as heart attack, stroke, and kidney failure. Treatment for hypertension may include lifestyle changes, such as diet and exercise, as well as medication.
Another disorder of the cardiovascular system is coronary artery disease (CAD). CAD occurs when the blood vessels that supply oxygen and nutrients to the heart become narrowed or blocked due to the buildup of plaque. This can result in chest pain, known as angina, and can eventually lead to a heart attack if the blood flow to the heart is completely blocked. Treatment for CAD may include lifestyle changes, medication, and procedures such as angioplasty or bypass surgery.
In addition to hypertension and CAD, there are many other disorders that can affect the cardiovascular system, including heart failure, arrhythmias, and valvular heart disease. Heart failure occurs when the heart is unable to pump enough blood to meet the body’s demands. Arrhythmias are abnormal heart rhythms that can range from harmless to life-threatening. Valvular heart disease occurs when the valves in the heart do not function properly, leading to problems with blood flow. Treatment for these disorders may vary depending on the specific condition, but may include medication, lifestyle changes, and procedures such as valve replacement or implantation of a pacemaker.
Gastrointestinal System Disorders
The gastrointestinal (GI) system consists of the organs responsible for the digestion and absorption of food, as well as the elimination of waste products. Disorders of the GI system can range from mild and temporary to severe and chronic. They can affect any part of the GI tract, including the esophagus, stomach, small intestine, large intestine, liver, gallbladder, and pancreas.
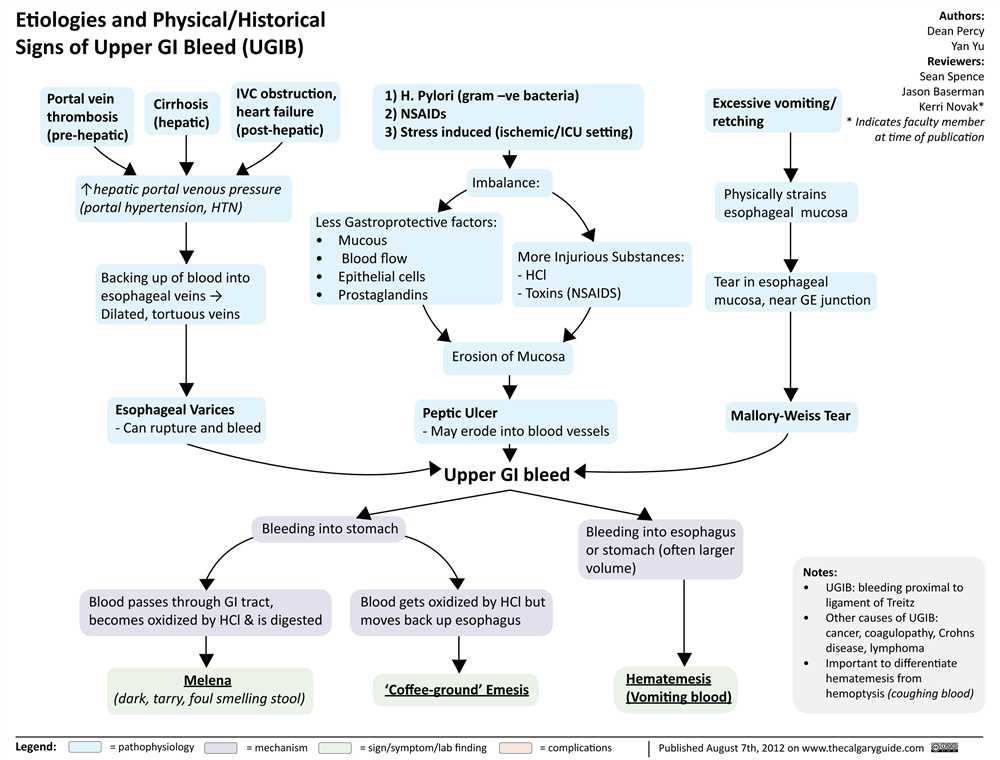
One common GI disorder is gastroesophageal reflux disease (GERD), which occurs when the contents of the stomach flow back into the esophagus, causing symptoms such as heartburn and regurgitation. Another is peptic ulcer disease, which is characterized by open sores in the lining of the stomach or duodenum. Other disorders include inflammatory bowel disease (IBD), which includes Crohn’s disease and ulcerative colitis, and irritable bowel syndrome (IBS), which is characterized by abdominal pain, bloating, and changes in bowel habits.
GERD: Gastroesophageal reflux disease (GERD) is a chronic condition in which the stomach acid flows back into the esophagus, causing irritation and discomfort. Common symptoms include heartburn, regurgitation, and chest pain. Lifestyle modifications and medications can help manage symptoms, but in severe cases, surgery may be necessary.
Peptic Ulcer Disease: Peptic ulcer disease is a condition characterized by open sores, or ulcers, in the lining of the stomach or duodenum. It is often caused by infection with Helicobacter pylori bacteria or by long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs). Symptoms may include abdominal pain, bloating, nausea, and vomiting. Treatment typically involves antibiotics to eradicate the bacterial infection, acid-suppressing medications to reduce stomach acid production, and lifestyle modifications.
- Inflammatory Bowel Disease: Inflammatory bowel disease (IBD) is a chronic autoimmune condition that causes inflammation in the lining of the digestive tract. Crohn’s disease and ulcerative colitis are the two main types of IBD. Symptoms include abdominal pain, diarrhea, weight loss, and fatigue. Treatment may include medication to control inflammation, dietary changes, and in severe cases, surgery to remove damaged portions of the intestine.
- Irritable Bowel Syndrome: Irritable bowel syndrome (IBS) is a functional disorder of the GI tract that is characterized by abdominal pain, bloating, and changes in bowel habits. The exact cause of IBS is unknown, but it is thought to be related to abnormal muscle contractions in the intestines. Treatment may include dietary modifications, stress management techniques, and medications to relieve symptoms.
There are many other disorders that can affect the gastrointestinal system, including liver disease, gallbladder disease, and pancreatic disorders. All of these conditions can cause a range of symptoms and may require different treatment approaches. It is important to consult with a healthcare professional for an accurate diagnosis and appropriate management of GI disorders.
Renal System Disorders
The renal system, also known as the urinary system, is responsible for regulating the balance of fluids, electrolytes, and acidity in the body. It includes the kidneys, ureters, bladder, and urethra. Disorders of the renal system can have a significant impact on overall health and well-being.
Renal failure is a serious condition in which the kidneys are unable to adequately filter waste products from the blood. There are two main types of renal failure: acute and chronic. Acute renal failure occurs suddenly and is often caused by a sudden drop in blood supply to the kidneys, a blockage in the urinary tract, or severe dehydration. Chronic renal failure, on the other hand, develops gradually over time and is usually the result of long-term conditions such as diabetes or high blood pressure.
Urinary tract infections (UTIs) are another common disorder of the renal system. UTIs occur when bacteria enter the urinary tract and multiply, causing inflammation and infection. Symptoms of a UTI may include pain or burning during urination, frequent urination, cloudy or bloody urine, and a strong odor. UTIs are typically treated with antibiotics.
Kidney stones are hard deposits that form in the kidneys. They can range in size from as small as a grain of sand to as large as a golf ball. Kidney stones are often caused by an imbalance in urine composition, such as high levels of calcium, oxalate, or uric acid. The most common symptom of kidney stones is severe pain in the side or back, which can radiate to the lower abdomen and groin. Treatment options for kidney stones include medication, lifestyle changes, and in some cases, surgical removal.
Polycystic kidney disease (PKD) is a genetic disorder that causes cysts to develop in the kidneys. These cysts can gradually enlarge, leading to kidney damage and eventually kidney failure. Other symptoms of PKD may include high blood pressure, back or abdominal pain, and recurrent urinary tract infections. Treatment for PKD focuses on managing symptoms and preventing complications.
Endocrine System Disorders
The endocrine system is responsible for regulating various physiological processes in the body through the release of hormones. However, disruptions in the normal functioning of the endocrine system can lead to the development of various disorders. These disorders may result from either an excessive or insufficient secretion of hormones.
One common endocrine disorder is diabetes mellitus, characterized by high blood sugar levels. There are two main types of diabetes mellitus: type 1 and type 2. Type 1 diabetes occurs when the body does not produce enough insulin, a hormone that helps regulate blood sugar levels. On the other hand, type 2 diabetes occurs when the body becomes resistant to insulin or does not use it effectively. Both types of diabetes can lead to serious complications if not properly managed.
Another example of an endocrine disorder is hypothyroidism, which occurs when the thyroid gland does not produce enough thyroid hormone. This condition can result in symptoms such as fatigue, weight gain, and cold intolerance. Hypothyroidism can be caused by autoimmune diseases, certain medications, or iodine deficiency.
Hyperthyroidism, on the other hand, is a condition characterized by excessive production of thyroid hormone. It can cause symptoms such as weight loss, increased heart rate, and irritability. One common cause of hyperthyroidism is Graves’ disease, an autoimmune disorder in which the immune system mistakenly attacks the thyroid gland.
Other endocrine disorders include Cushing’s syndrome, characterized by excessive production of cortisol hormone; Addison’s disease, which occurs when the adrenal glands do not produce enough cortisol and aldosterone; and polycystic ovary syndrome (PCOS), a hormonal disorder that affects women and can cause irregular periods and infertility.
Summary:
- The endocrine system is responsible for regulating physiological processes through the release of hormones.
- Disorders of the endocrine system can result from either excessive or insufficient hormone secretion.
- Examples of endocrine disorders include diabetes mellitus, hypothyroidism, hyperthyroidism, Cushing’s syndrome, Addison’s disease, and polycystic ovary syndrome (PCOS).