For successful completion of the Advanced Cardiovascular Life Support (ACLS) exam, understanding key protocols is non-negotiable. Focus on the primary assessment steps: check responsiveness, initiate chest compressions, and manage the airway as needed. You must be ready to respond to arrhythmias by using the appropriate drugs and electrical therapies, such as defibrillation for shockable rhythms and medication management for non-shockable rhythms.
Pay attention to the following critical scenarios: In cases of cardiac arrest, knowing the correct drug administration intervals is key. Ensure you are familiar with the recommended doses for epinephrine, amiodarone, and other critical medications. The timing of each step, from chest compressions to defibrillation, plays a significant role in the survival outcome.
Advanced airway management: While securing the airway, be mindful of techniques like endotracheal intubation or supraglottic airway placement. Also, familiarize yourself with the use of capnography to assess endotracheal tube placement. Early oxygenation and ventilation can make a substantial difference in patient prognosis.
Post-cardiac arrest care: Understand the importance of stabilizing the patient and monitoring for potential complications like arrhythmias or hypotension. The post-resuscitation phase involves managing the airway, optimizing hemodynamics, and considering targeted temperature management (TTM) if indicated.
Practice these critical skills regularly: ACLS exams are based on scenarios that require quick decision-making under pressure. The more you rehearse the protocols, the better prepared you’ll be when the moment comes. Be confident in your ability to follow each step with precision.
Sure! Here’s a detailed plan for the article titled “Advanced Cardiovascular Life Support Exam A Answers” in HTML format, focusing on specific and practical aspects:
For the Advanced Cardiovascular Life Support (ACLS) Exam A, focus on these key areas to enhance your understanding and improve exam performance:
Cardiac Arrest Management
Immediately assess the patient for signs of cardiac arrest. If absent, begin high-quality chest compressions without delay:
- Follow the 30:2 compression-to-ventilation ratio for adults.
- Use an AED (Automated External Defibrillator) as soon as available.
- Administer epinephrine every 3-5 minutes during resuscitation.
- Consider advanced airway management after 2 minutes of resuscitation.
Pharmacology and Drug Administration
In ACLS, certain medications are crucial for effective treatment during cardiac emergencies:
- Administer atropine for bradycardia when the heart rate is below 60 bpm and symptomatic.
- Administer amiodarone after the third shock for shock-refractory ventricular fibrillation.
- Epinephrine is used for both cardiac arrest and anaphylactic shock, improving myocardial perfusion.
Airway Management
Secure the airway and optimize ventilation:
- Use a bag-valve mask for non-invasive ventilation, ensuring an airtight seal.
- Consider intubation for patients unresponsive to initial measures.
- Ensure that oxygen saturation remains above 94% to prevent hypoxia.
Post-Resuscitation Care
After restoring a pulse, focus on stabilizing the patient:
- Begin targeted temperature management (TTM) to prevent neurological damage.
- Monitor ECG for arrhythmias and treat accordingly.
- Establish IV access for continued drug administration and fluid resuscitation.
Focusing on these actions and understanding the corresponding drug dosages, compression techniques, and timing will aid in achieving success on the ACLS Exam A. Prioritize critical interventions, always following the most up-to-date guidelines for the best outcomes.
Understanding Key Concepts of ACLS Algorithms
Follow the ACLS algorithms step-by-step, prioritizing high-quality chest compressions and early defibrillation when indicated. Recognize the importance of early access to advanced care and ensure the correct medication is administered according to the rhythm and condition of the patient. Focus on maintaining high-quality CPR throughout the process and avoid unnecessary interruptions.
Basic Life Support (BLS) Integration
Before initiating ACLS interventions, ensure BLS is performed. Chest compressions should be at least 2 inches deep at a rate of 100-120 compressions per minute. Always begin with an initial assessment of the airway, breathing, and circulation (ABCs) and ensure early defibrillation is available. After the initial BLS steps, proceed with more advanced interventions such as medications or advanced airway management if necessary.
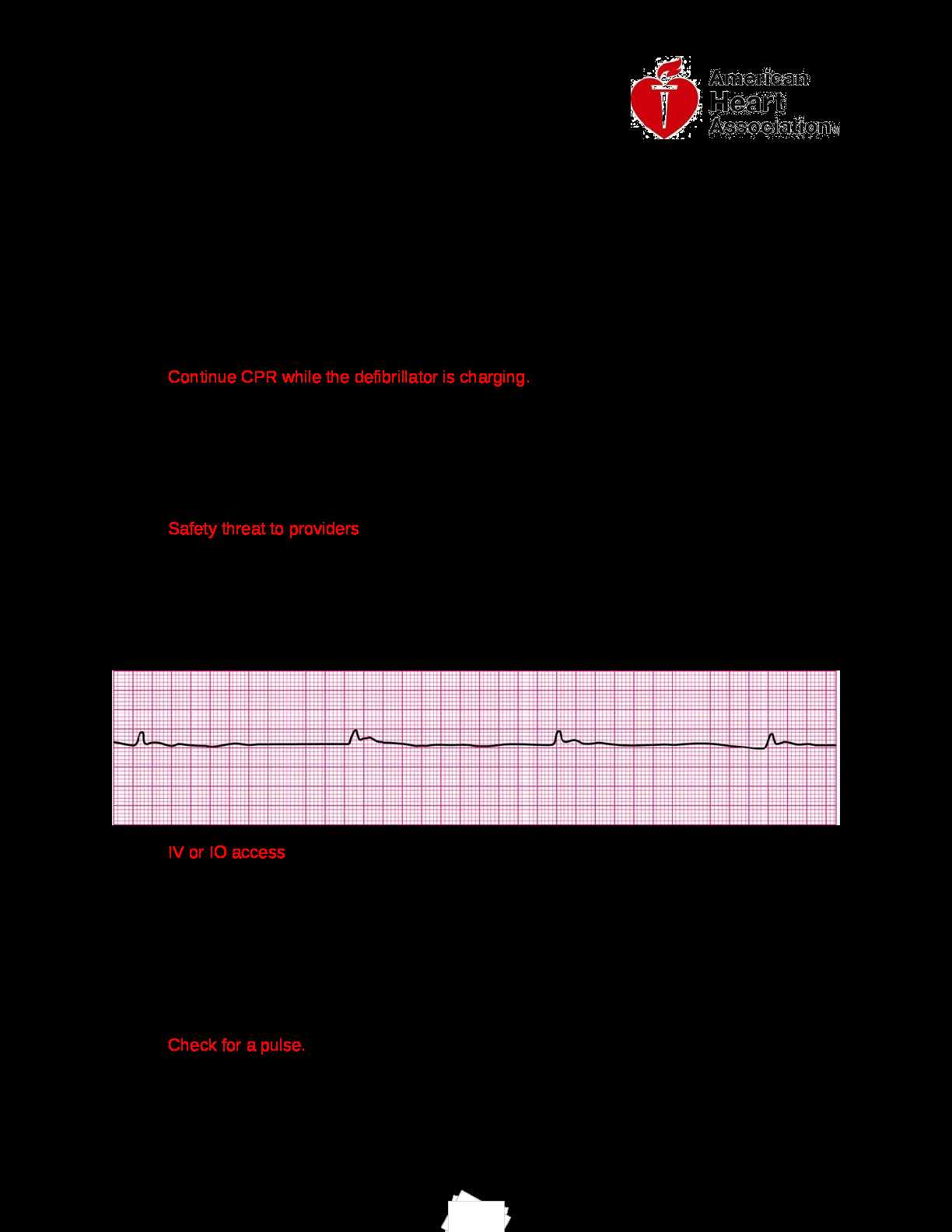
Rhythm-Based Approaches
ACLS algorithms are centered around identifying the rhythm of the patient’s heart to determine appropriate interventions. In cases of shockable rhythms, such as ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT), immediate defibrillation is required. For non-shockable rhythms, like asystole or pulseless electrical activity (PEA), continue with CPR while addressing the underlying causes.
Interpreting Common Scenarios in the Exam
In a scenario where a patient shows signs of acute respiratory distress, immediately assess the airway and breathing. Ensure that the airway is clear and begin bag-valve-mask ventilation if necessary. This will support oxygenation until more advanced interventions are possible.
For cases of shock, prioritize fluid resuscitation. If the patient’s blood pressure drops significantly and they show signs of hypoperfusion, start with a bolus of normal saline or lactated Ringer’s solution, and monitor closely for improvements in vital signs. Always consider a differential diagnosis of causes of shock such as hypovolemic, cardiogenic, or distributive shock.
If a patient presents with a sudden cardiac arrest, follow the algorithm for high-quality chest compressions, defibrillation (if indicated), and early advanced cardiac life support. Use epinephrine every 3-5 minutes during the resuscitation phase, and administer amiodarone or lidocaine if the rhythm is shock-resistant.
In situations involving a bradycardic patient, assess if atropine is appropriate for symptomatic bradycardia. If the heart rate is extremely low and the patient is hemodynamically unstable, atropine can be used to increase the heart rate. If atropine is ineffective, prepare for pacing or consider using dopamine or epinephrine drips.
For arrhythmias such as ventricular tachycardia or atrial fibrillation, it’s crucial to differentiate between stable and unstable conditions. In unstable arrhythmias, synchronized cardioversion should be performed immediately. For stable conditions, pharmacological therapy such as antiarrhythmic medications may be appropriate, depending on the patient’s clinical status.
Preparing with Practice Questions for ACLS
Focus on solving practice questions that reflect the structure and content of the ACLS exam. Answering realistic questions helps you understand the format and pinpoint areas that need more attention. Make sure to review your mistakes and understand why the correct answers are right. This will enhance your problem-solving skills and boost confidence.
Simulate Exam Conditions
Set aside time to answer practice questions under timed conditions. Mimicking the real exam environment helps manage time effectively and builds mental stamina for the test. By simulating pressure, you’ll become more comfortable with the pace of the exam.
Review Guidelines and Algorithms
ACL guidelines and algorithms are key to the exam. Ensure you’re familiar with the latest protocols and how they apply to specific clinical scenarios. Practice questions often test your ability to recall and apply these algorithms correctly in high-stress situations. By continuously practicing, you’ll improve your recall speed and accuracy.