Introduction: The Attest Biological Indicator is a crucial tool in the field of sterilization. It is used to validate the effectiveness of sterilization processes and to ensure the safety of medical instruments and devices. These instructions provide a step-by-step guide on how to use and interpret the results of the Attest Biological Indicator.
Step 1: Preparation: Before using the Attest Biological Indicator, make sure to read and understand the product instructions. Gather all the necessary materials, including the Attest Biological Indicator, an incubator, and a sterilization cycle record. Ensure that the incubator and sterilization equipment are clean and in good working condition.
Step 2: Testing: To perform the test, expose the Attest Biological Indicator to the sterilization process. This can be done by placing the indicator in the same location as the medical instruments being sterilized. Make sure to adhere to the recommended temperature, pressure, and time parameters for the sterilization process.
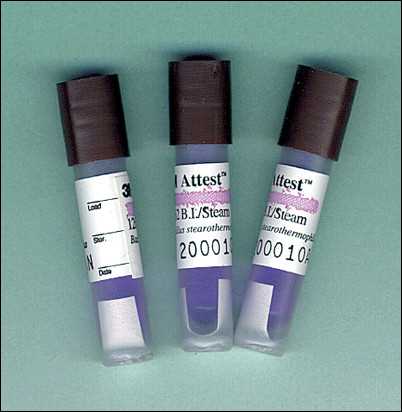
Step 3: Incubation: After the sterilization process is complete, transfer the Attest Biological Indicator to the incubator. The incubator should be set to the appropriate temperature for the specified incubation time. It is crucial to follow the recommended incubation time to ensure accurate results. During this time, the indicator will undergo a color change, indicating whether or not the sterilization process was successful.
Step 4: Result interpretation: Once the incubation period is over, it is time to interpret the results. A color change to yellow indicates a positive result, meaning that the biological indicator has been sterilized successfully. If the indicator remains purple, it means that the sterilization process did not eliminate all the biological contaminants, and further action may be required.
Conclusion: The Attest Biological Indicator Instructions provide a systematic approach to validate and verify the effectiveness of sterilization processes. By following these instructions, healthcare professionals can ensure the safety and efficacy of their medical instruments and devices, promoting overall patient well-being.
Understanding the importance of Attest biological indicators
Attest biological indicators are an essential tool in ensuring the effectiveness of sterilization processes in healthcare settings. These indicators, which contain a known population of highly resistant microorganisms, are used to monitor the performance of sterilizers and validate the efficacy of the sterilization cycle. By using Attest biological indicators, healthcare facilities can have confidence that their sterilization processes are working effectively, minimizing the risk of healthcare-associated infections.
One key advantage of Attest biological indicators is their ability to provide a direct measurement of microbial inactivation. Unlike other sterilization monitoring methods, such as chemical indicators or integrators, Attest biological indicators can confirm whether or not the sterilization process has actually killed the microorganisms present in the test load. This ensures that the process is achieving the intended level of microbial reduction, which is crucial for preventing the transmission of pathogens in healthcare settings.
Using Attest biological indicators as part of a comprehensive sterilization monitoring program can help healthcare facilities comply with regulatory requirements and industry standards. It is essential for healthcare providers to demonstrate that their sterilization processes are being properly monitored and validated, and the use of Attest biological indicators is an important component of this.
Implementing an effective sterilization monitoring program with Attest biological indicators can also help healthcare facilities improve patient safety and quality of care. By ensuring that sterilization processes are consistently effective, healthcare-associated infections can be minimized, leading to improved patient outcomes and reduced healthcare costs.
In conclusion, understanding the importance of Attest biological indicators is crucial for healthcare facilities. These indicators provide a direct measurement of microbial inactivation, help comply with regulatory requirements, and improve patient safety. By using Attest biological indicators, healthcare providers can have confidence in the effectiveness of their sterilization processes, ultimately leading to better outcomes for patients.
Step-by-step guidelines for using Attest biological indicators
Attest biological indicators are an essential tool for ensuring the efficacy of sterilization processes in healthcare settings. Proper usage of these indicators is crucial to maintain the safety and effectiveness of medical equipment and instruments. Here are step-by-step guidelines for using Attest biological indicators.
1. Prepare the sterilization equipment
Before using the Attest biological indicators, ensure that the sterilization equipment, such as an autoclave or ethylene oxide sterilizer, is set up and functioning properly. Follow the manufacturer’s instructions for the specific sterilization equipment being used.
2. Incorporate Attest biological indicators into the load
Place the Attest biological indicators in strategic locations within the load, such as near the center or in hard-to-reach areas. This ensures that the indicators are exposed to the same conditions as the instruments or equipment being sterilized. Secure the biological indicators in a way that prevents them from moving or shifting during the sterilization process.
3. Run the sterilization cycle
Initiate the sterilization cycle according to the recommended parameters for the specific sterilization equipment being used. It is essential to follow the recommended time, temperature, and pressure settings to achieve proper sterilization. Monitor the sterilization process closely to ensure that it runs smoothly and without any interruptions.
4. Monitor the biological indicators
During the sterilization cycle, closely monitor the Attest biological indicators to ensure that they are exposed to the sterilization conditions. Observe the color change or other indicators provided by the Attest biological indicators to determine the presence of live biological spores. Any deviation from the expected results could indicate a potential sterilization failure.
5. Interpret the results
After the sterilization cycle is complete, carefully interpret the results of the Attest biological indicators. If the indicator shows no growth or change in color, it indicates a successful sterilization process. However, if there is growth or any deviation from the expected results, it indicates a sterilization failure, and the load should not be used until reprocessed.
6. Record the results
Document the results of the Attest biological indicators for compliance and record-keeping purposes. Include the date, time, sterilization cycle parameters, and the results of the biological indicators. This documentation is essential for audit purposes and ensuring quality assurance in sterilization processes.
By following these step-by-step guidelines for using Attest biological indicators, healthcare professionals can ensure the effectiveness of sterilization processes and maintain the highest level of safety for patients and healthcare workers.
Tips for Interpreting Attest Biological Indicator Results
The Attest biological indicator is a crucial tool for monitoring the effectiveness of sterilization processes. Interpreting the results correctly is essential to ensure the safety and efficacy of medical devices and equipment. Here are some tips to help you interpret Attest biological indicator results:
1. Familiarize Yourself with the Control
Before interpreting the results, it’s essential to understand the control indicator included with the Attest biological indicator. The control serves as a reference point to ensure that the sterilization process was effective. If the control shows growth, it indicates that the sterilization process was inadequate or the biological indicator was contaminated. Therefore, always check the control first before interpreting the results.
2. Look for Color Change
The Attest biological indicator consists of a media vial and a color-changing strip. A color change from the initial purple to yellow indicates a positive result, indicating that the sterilization process was successful in killing the spores. However, if the strip remains purple or shows a different color change, it suggests that the sterilization process may not have been effective. In such cases, further investigation and re-sterilization may be necessary.
3. Consider Incubation Time
It’s crucial to follow the recommended incubation time provided by the manufacturer. The incubation period allows any surviving spores to grow, making it easier to detect their presence. If the incubation time is insufficient, the results may not be accurate, leading to incorrect interpretations. Ensure that you adhere to the specified incubation period to obtain reliable results.
4. Consult the Manufacturer’s Instructions
Each Attest biological indicator may have specific instructions and guidelines provided by the manufacturer. It’s important to consult these instructions and follow them meticulously. The manufacturer’s guidance will provide valuable information on how to handle and interpret the results accurately. Failure to follow the instructions may compromise the validity of the results and affect the reliability of the sterilization process.
Interpreting Attest biological indicator results requires attention to detail and adherence to the specific instructions provided. By familiarizing yourself with the control, observing color changes, considering the incubation time, and following the manufacturer’s instructions, you can ensure accurate interpretation and maintain a safe and effective sterilization process for medical devices and equipment.
Common Mistakes to Avoid When Using Attest Biological Indicators
When using Attest biological indicators, it is important to follow the instructions carefully to ensure accurate and reliable results. However, there are some common mistakes that users may make. By being aware of these mistakes, you can minimize the risk of improper usage and potential errors.
1. Not properly preparing the biological indicator:

One common mistake is not properly preparing the biological indicator before use. This can include failure to activate the indicator or not allowing it enough time to reach the appropriate temperature. It is crucial to carefully read the instructions and follow the recommended activation and incubation times to ensure that the biological indicator is ready for use.
2. Neglecting to perform a control test:
Another common mistake is neglecting to perform a control test alongside the biological indicator. A control test is a critical step in validating the sterilization process. This test serves as a baseline to confirm that the indicator is functioning correctly and that the sterilization process has been effective. Failure to perform a control test can lead to inaccurate results and a false sense of security.
3. Failing to interpret the results correctly:
Interpreting the results of the biological indicator is essential for determining the effectiveness of the sterilization process. However, not understanding how to interpret the results correctly can lead to confusion or misinterpretation. It is crucial to familiarize yourself with the recommended interpretation guidelines and seek clarification if you are uncertain about the results.
To avoid these common mistakes, it is crucial to thoroughly read and understand the instructions provided by the manufacturer. Following the instructions precisely and conducting necessary control tests will help ensure accurate and reliable results when using Attest biological indicators.
Ensuring accurate and reliable results with Attest biological indicators

In order to ensure accurate and reliable results when using Attest biological indicators, it is important to follow the instructions provided by the manufacturer. These instructions are designed to optimize the performance of the indicator and to ensure that the results obtained are valid and meaningful.
The following key points should be considered when using Attest biological indicators:
- Follow the instructions: It is essential to carefully read and understand the instructions provided by the manufacturer. This includes information on how to properly use the indicator, how to interpret the results, and any additional precautions or recommendations.
- Proper storage and handling: Attest biological indicators should be stored in a cool and dry place, away from direct sunlight and chemicals that may affect their performance. Additionally, it is important to handle the indicators with clean hands and to avoid any contamination that may compromise the results.
- Correct incubation conditions: The incubation conditions, including temperature and time, should be strictly followed as specified in the instructions. Deviating from these conditions may result in inaccurate or unreliable results.
- Regular quality control: It is recommended to perform regular quality control checks on the biological indicators to ensure their performance and reliability. This can be done by following the provided guidelines for positive and negative controls.
- Record keeping: It is essential to maintain a record of each biological indicator test performed, including the date, time, test results, and any relevant notes. This record will serve as a reference for future assessments and audits.
By following these guidelines and ensuring strict adherence to the instructions provided, you can enhance the accuracy and reliability of your results when using Attest biological indicators. This will ultimately contribute to the overall effectiveness of your sterilization processes, ensuring a safe and controlled environment.
Q&A:
What are Attest biological indicators?
Attest biological indicators are specialized tools used to monitor the efficacy of sterilization processes in healthcare settings. They contain specific microorganisms that are resistant to the sterilization methods and are used to challenge the process.
How do Attest biological indicators work?
Attest biological indicators work by containing a population of microorganisms that are known to be resistant to the sterilization process being monitored. The indicator is placed inside the sterilization chamber along with the items being sterilized. After the sterilization cycle is complete, the indicator is incubated and observed for any growth of the resistant microorganisms. If no growth is observed, it indicates that the sterilization process was effective.
Why is it important to use Attest biological indicators?
Using Attest biological indicators is important to ensure the accuracy and reliability of sterilization processes. They provide a direct measure of the effectiveness of the sterilization process by challenging it with resistant microorganisms. This helps to detect any failures in the process and allows for necessary corrective actions to be taken.
What types of sterilization processes can Attest biological indicators be used for?
Attest biological indicators can be used for various types of sterilization processes, including steam, ethylene oxide, hydrogen peroxide, and dry heat sterilization. Each type of sterilization method requires a specific biological indicator that is resistant to the particular process.
How often should Attest biological indicators be used?
The frequency of using Attest biological indicators depends on the regulatory requirements and the specific healthcare facility’s sterilization protocols. Generally, biological indicators should be used with every load or at least once a day to ensure the ongoing effectiveness of the sterilization processes.