To manage hypertension and type 2 diabetes together, focus on a holistic approach that addresses both conditions simultaneously. Consistent monitoring of blood pressure and blood sugar levels is the cornerstone of this strategy. Patients should aim to maintain blood pressure below 130/80 mm Hg and target an HbA1c of 7% or lower, depending on individual circumstances.
Diet plays a significant role. A balanced, low-sodium diet rich in whole grains, vegetables, lean proteins, and healthy fats can reduce hypertension. At the same time, managing carbohydrate intake and emphasizing fiber-rich foods helps in controlling blood glucose levels. This combined dietary approach improves overall cardiovascular health and metabolic control.
Physical activity is another key factor in managing both conditions. Regular aerobic exercise, such as walking or swimming, can lower blood pressure and improve insulin sensitivity. Aim for at least 150 minutes of moderate-intensity exercise per week. Strength training exercises twice a week also provide additional benefits, including improved muscle mass and better glucose metabolism.
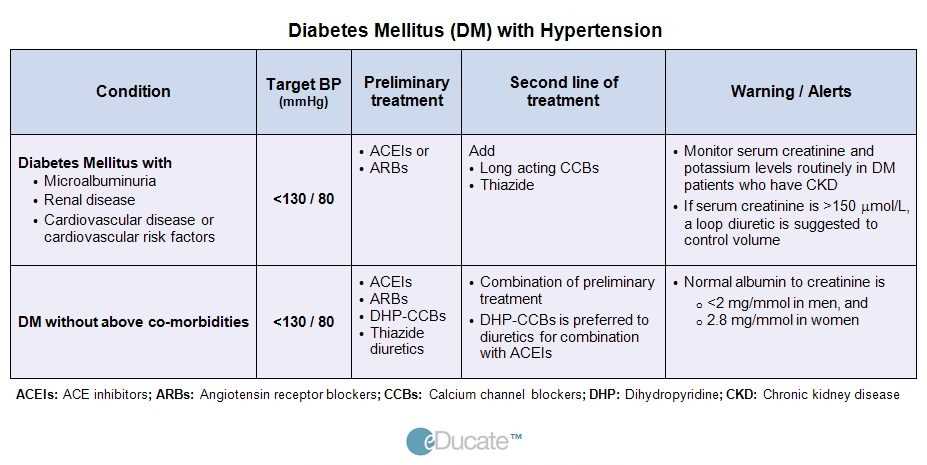
Medication adherence is essential. Angiotensin-converting enzyme (ACE) inhibitors, calcium channel blockers, and diuretics can be prescribed to control hypertension. For type 2 diabetes, metformin remains the first-line treatment, with additional medications like SGLT2 inhibitors or GLP-1 agonists if necessary. Combining these medications effectively requires regular follow-ups to monitor for side effects and adjust dosages accordingly.
Shadow Health Focused Exam Hypertension and Type 2 Diabetes Answers
Monitor blood pressure regularly. For patients with hypertension, maintaining readings below 140/90 mmHg is recommended. Lifestyle modifications, such as reducing sodium intake, increasing physical activity, and managing stress, are key to controlling blood pressure. Medications like ACE inhibitors, calcium channel blockers, or diuretics may be prescribed depending on the severity of hypertension.
Management of Hypertension in Diabetic Patients
In patients with both hypertension and type 2 diabetes, blood pressure control is vital to reduce the risk of cardiovascular complications. Focus on achieving a target below 130/80 mmHg. Angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs) are particularly beneficial for diabetic patients due to their protective effects on the kidneys. Regular kidney function tests should be performed to monitor for any signs of diabetic nephropathy.
Type 2 Diabetes Management
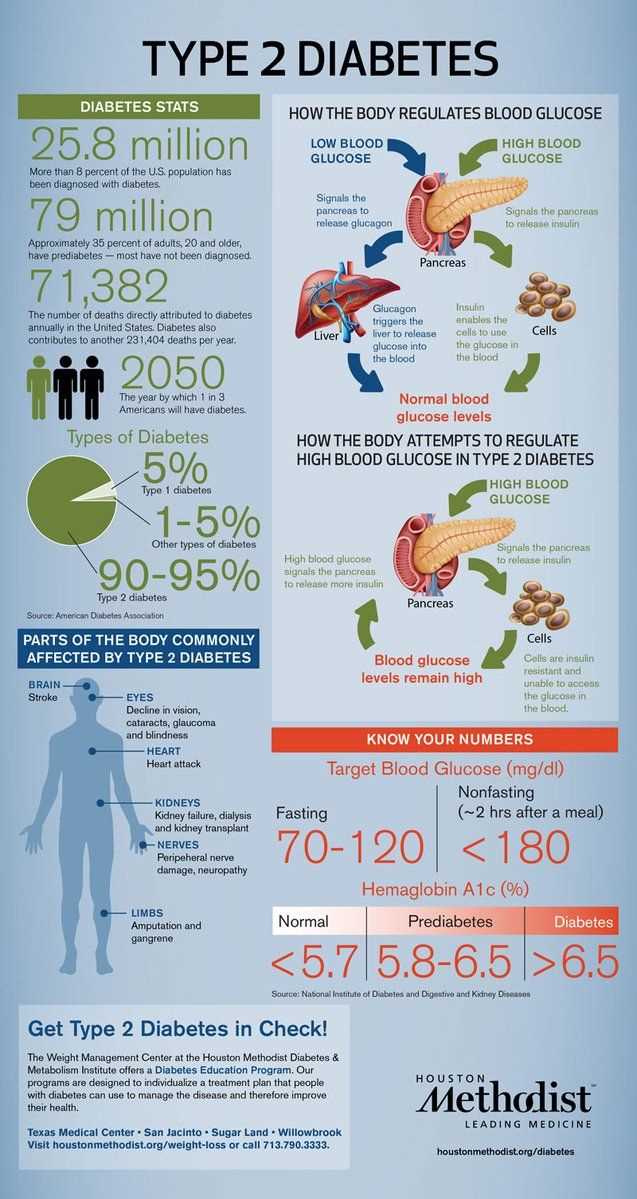
For managing type 2 diabetes, focus on controlling blood sugar levels within a range of 70–130 mg/dL before meals. Encourage a balanced diet, rich in fiber and low in refined sugars, alongside regular physical activity. Medications like metformin are commonly prescribed to improve insulin sensitivity. If needed, other medications such as sulfonylureas, DPP-4 inhibitors, or GLP-1 receptor agonists may be considered. Regular monitoring of HbA1c levels should be conducted to evaluate long-term glucose control.
Patient education on self-management is essential. Encourage the use of home blood glucose monitors to track daily levels, ensuring better control. Regular follow-ups are crucial to adjust treatment plans as needed, with close attention to potential complications such as diabetic retinopathy or neuropathy.
Managing Blood Pressure in Patients with Type 2 Diabetes
Achieving optimal blood pressure control is key for patients with type 2 diabetes to reduce the risk of cardiovascular events. Aim for a target of less than 140/90 mmHg, though more stringent targets (e.g., <130/80 mmHg) may benefit some individuals with additional risk factors.
Begin with lifestyle modifications, focusing on weight loss, increased physical activity, and a heart-healthy diet. The DASH (Dietary Approaches to Stop Hypertension) diet, rich in fruits, vegetables, and low-fat dairy, is particularly beneficial. Limiting sodium intake and moderating alcohol consumption also contribute to better blood pressure control.
Pharmacological treatment often complements lifestyle changes. Common medications for these patients include ACE inhibitors, angiotensin II receptor blockers (ARBs), and calcium channel blockers. These not only lower blood pressure but also offer kidney protection, which is critical for diabetic patients who may be at risk of nephropathy.
Monitor renal function regularly, as some antihypertensive medications can impact kidney function. Adjust treatment as needed, keeping in mind the patient’s overall health status, comorbidities, and any adverse effects from medication.
Incorporating a team approach with primary care providers, endocrinologists, and dietitians ensures that blood pressure management remains comprehensive and individualized, improving outcomes for patients with type 2 diabetes.
Common Challenges in Diagnosis and Treatment of Hypertension in Diabetic Patients
Accurate diagnosis of hypertension in diabetic patients often proves difficult due to overlapping symptoms of both conditions. Blood pressure measurements must be taken consistently, considering that the presence of elevated glucose levels can contribute to falsely high readings. Routine monitoring should be more frequent to ensure precise detection, especially in patients with poorly controlled blood sugar.
Medication Interactions and Side Effects
Choosing antihypertensive medication for diabetic patients requires careful consideration of potential drug interactions. Some medications, such as beta-blockers, may mask hypoglycemia symptoms, making it harder to manage blood sugar levels. Additionally, certain diuretics can worsen kidney function, which is a concern in diabetic patients prone to nephropathy. Always monitor kidney function closely when prescribing these drugs and consider alternatives like ACE inhibitors or angiotensin II receptor blockers, which have protective effects on the kidneys.
Managing Comorbidities
Hypertension and diabetes often coexist with other health issues, such as obesity and dyslipidemia. These comorbidities complicate treatment plans, as lifestyle modifications and dietary changes are crucial for both conditions. Encourage patients to follow heart-healthy diets, exercise regularly, and adhere to glucose control measures. In many cases, a multi-disciplinary approach involving a dietitian, endocrinologist, and cardiologist provides the best results.
Monitoring and Adjusting Treatment for Long-Term Health Outcomes
Regular monitoring of blood pressure and blood glucose levels is key for managing hypertension and type 2 diabetes. Patients should have their blood pressure checked at least every 3-6 months and blood glucose levels assessed according to their individual treatment plan.
Adjusting treatment plans based on these readings helps prevent complications. For hypertension, aim for a target blood pressure of less than 140/90 mmHg, and for type 2 diabetes, maintain an HbA1c level below 7%. When either of these targets is not met, medications may need to be changed or doses altered.
- Blood pressure medications, such as ACE inhibitors or ARBs, may be adjusted if readings consistently exceed targets.
- Insulin therapy for diabetes can be intensified or changed to a different regimen if blood glucose control is suboptimal.
- Adding lifestyle interventions, like diet changes and increased physical activity, can significantly enhance long-term outcomes.
Regular blood tests, including kidney function tests and lipid profiles, also play a role in adjusting treatment. If kidney function declines, the use of certain antihypertensive drugs may need to be reconsidered.
Patient adherence to medications and lifestyle changes directly impacts treatment success. Educating patients on the importance of consistent treatment and lifestyle modifications is vital for achieving long-term health outcomes.
- Routine follow-up appointments help assess adherence and make necessary adjustments.
- Collaborating with a healthcare team, including dietitians and endocrinologists, ensures a well-rounded approach to treatment.
Maintaining open communication with patients allows for early identification of complications, making it easier to adjust treatment in a timely manner. Early intervention significantly reduces the risk of long-term complications like heart disease, stroke, and kidney failure.